Gastric cancer
Gastric cancer is a cancer of the stomach wall that is currently the fourth leading cause of cancer death in Europe. It is the second most common malignant disease worldwide. Gastric cancer develops through a complex multistage process with several distinct histological and pathophysiological phases. The whole development is influenced by a complex of interactions between bacteria, the environment, the genetic dispositions of the host and molecular mechanisms. Many of the etiologies and pathogenesis of this disease remain unclear, but the underlying context is already known.
Epidemiology[edit | edit source]
Gastric cancer is an exception among cancers, as its incidence and mortality have decreased significantly in the last 25 years. The incidence decreased by about one third and the mortality due to improved therapeutic options by up to half. We can observe a completely opposite trend in colorectal cancer, the incidence of which, on the other hand, is still rising and our country is one of the world's leading figures.[1]
The highest incidence in each country shows the highest incidence in Japan and Asian countries, allegedly due to the high content of nitrosamines and nitrosamides in fish feed. In the Czech Republic, the incidence reaches 15: 100,000 inhabitants (according to IHIS CR).[2]
Men are more often affected than women and the risk increases gradually with age, with the highest incidence at 70-74 years.
Etiology of gastric cancer[edit | edit source]
It varies according to the histological type of the tumor. According to Lauren's classification, we distinguish between intestinal and diffuse types. The intestinal type is most often caused by H. pylori infection , exposure to carcinogens from food and tobacco smoke, and many other factors. Although gastric adenocarcinoma is sporadic in the vast majority of cases, there are also familial forms, mainly associated with the diffuse type . [3]
The main risk factors include:
- smoking and consumption of hard alcohol,
- dietary carcinogens (smoking, salting, nitrosamines, polyaromatic hydrocarbons - PAHs),
- chronic diseases:
- atrophic gastritis,
- Menetrier's disease,
- achlorhydria,
- pernicious anemia,
- gastroesophageal reflux,
- gastric resection II. type (especially the area of anastomoses).
- polyposis adenomas,
Gastric polyps, if they do not have villous structures, are not considered precancerous lesions, however, it is recommended to remove all polyps larger than 2 cm, as the risk of villous structures and thus malignancy increases with size.
- infection by H. pylori
- For more information, see The role of Helicobacter pylori in the pathogenesis of gastric cancer
Symptomatology[edit | edit source]
The initial symptomatology of the disease is very non-specific (pain and pressure in the epigastrium, anorexia, weight loss, weakness, fatigue, nausea, belching, bad breath). Passage disorders can also occur, usually manifested by more frequent vomiting . Enlargement is manifested by enlarged left supraclavicular nodes (Virchow-Troisier) and ascites.
In advanced stages, there are dominant manifestations of complications:
- bleeding into the GIT – - mostly occult, it can also manifest as melena,
- pylorostenosis - followed by cachexia,
- perforation – peritonitis,
- fistula between stomach and colon transversum - malnutrition from protein loss,
- cardiac obstruction dysphagia.
Diagnosis[edit | edit source]
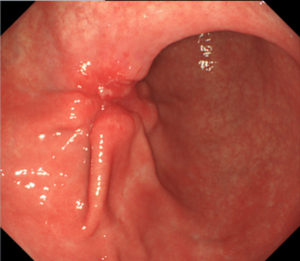
A patient with the symptomatology mentioned above should be consulted at the outpatient clinic of a gastrointestinal doctor who will perform a basic examination ( anamnesis and physical examination ). From the physical examination, we can observe, if present, palpable nodal metastases above the left collarbone (Virchow's node). The basic examination leading to the confirmation or refutation of the diagnosis of gastric cancer is endoscopic examination (gastroscopy), during which we take a multiple biopsy sample for histological verification of the finding. We can also perform cytology of gastric contents or endosonography.
In case of a positive histological finding, we always perform CT of the patient's abdomen , in cardiac and CT mediastinal tumors, in order to assess the size and location of the tumor and its growth through the stomach wall, or into other structures and infiltration of lymph nodes. We also note metastatic infiltration of other organs (especially the liver), if present. In women, we think of a possible metastatic ovarian disease (Krukenberg tumor). As part of pre-treatment staging, we also perform lung X-rays .
Based on the histological findings and CT, the team of gastroenterologist, surgeon and clinical oncologist determines the treatment options for the patient.
From other examinations we perform:
- Stomach X-ray or X-ray with contrast agent,
- blood test
- blood count – we can find signs of microcytic hypochromic anemia in corneal bleeding
- tumor markers (CEA, CA 19-9, CA72-4) – rather than the diagnostic effect, these values are used to evaluate the success of subsequent treatment and further course of the disease,
- liver ultrasonography to detect metastases,
- bone scintigraphy.
Pathology of gastric cancer[edit | edit source]
Gastric carcinoma (more precisely, adenocarcinoma) is the most common neoplasia of the stomach wall. The Lauren classification distinguishes between two types of gastric cancers, diffuse and intestinal.
The diffuse type is usually associated with an unfavorable prognosis, as it often shows a strong tendency to invade the surrounding tissue. Tumor cells of this type lose cohesion and original function. Compared to the intestinal type, its pathogenesis is much less studied.
The intestinal type has well-defined stages of development and tumor cells form into functional glands of the gastrointestinal tract.
For more information, see Pathology of gastric adenocarcinoma.
Therapy[edit | edit source]
The only potentially curative method of treatment is partial or complete gastrectomy . In addition, endoscopic resection , chemotherapy and radiotherapy are used . An important component of caring for a patient with gastric cancer is palliative care and the provision of adequate nutrition due to the high risk of cachectization.
Endoscopy[edit | edit source]
The endoscopic solution can be used both in very early stages of the disease (carcinoma in situ, T1), when we perform mucosectomies, and in very advanced tumors, when we palliatively apply stents to maintain cardiac patency.
Surgery[edit | edit source]
Surgical treatment is most important for low radiosensitivity. However, patients often come in late stages with an inoperable tumor (then only a palliative procedure supplemented by adjuvant chemo- and/or radiotherapy):
- gastrectomy with lymphadenectomy, omentectomy, event. with splenectomy;
- palliative gastroenteroanastomosis to maintain patency.
Sufficient radical surgery is necessary for the success of the treatment, a resection line 5-6 cm from the tumor is required. Resection of liver metastases does not affect survival.
Type of surgery:
- antrum tumor: subtotal gastrectomy;
- tumor in the stomach body: total or subtotal gastrectomy (according to location - 5 cm resection line required);
- tumor in the fundus: fundectomy (proximal 2/3 gastric resection) or total gastrectomy (according to tumor size and nodal involvement).
Chemotherapy[edit | edit source]
Palliative or adjuvant, eg. FAM (5-fluorouracil, adriamycin, mitomycin C), FAMtx (5-FU, adriamycin, methotrexate), FAB (5-FU, adriamycin, carmustine). More recently, the combination of EAP (etoposide, adriamycin, cisplatin), is preferred , which has a higher therapeutic response, but also higher toxicity.
Radiotherapy[edit | edit source]
Only palliatively in inoperable carcinomas ( however, in lymphomas it can lead to complete remission), brachyradiotherapy in the GE area to maintain patency. We use radiation at a dose of 40-45 Gy. The limit of the dose used is mainly the surrounding structures (kidneys, small intestine, liver, spinal cord).
Neoadjuvant concomitant chemoradiotherapy (5FU + irradiation) is now used at some foreign workplaces, which helps to reduce the tumor and thus improve its operability.
Targeted therapy[edit | edit source]
Trastuzumab treatment is indicated for palliative treatment of HER2 receptor overexpressing gastric adenocarcinoma (10-25% of tumors) . [4]
Prognosis[edit | edit source]
The prognosis for five-year survival is about 90% in clinical stage Ib, about 20% in stage IV (M0). More advanced forms are almost always infamous. In case of disease recurrence after surgery, few patients survive one year.
Literature[edit | edit source]
Related articles[edit | edit source]
- Gastroduodenal ulcer disease
- Stomach tumors
- Determination of antibodies against Helicobacter pylori
- Helicobacter pylori
- Pathology of gastric adenocarcinoma
Reference[edit | edit source]
- ↑ JAN ŽALOUDÍK Karcinom žaludku: DOPORUČENÉ POSTUPY PRO PRAKTICKÉ LÉKAŘE [online]. In: . Česká lékařská společnost Jana Evangelisty Purkyně, 2016 [cit. 2016-4-23]. Dostupné z: www.cls.cz/dokumenty2/os/r103.rtf
- ↑ DUŠEK Ladislav, MUŽÍK Jan, KUBÁSEK Miroslav, KOPTÍKOVÁ Jana, ŽALOUDÍK Jan, VYZULA Rostislav. Epidemiologie zhoubných nádorů v České republice [online]. Masarykova univerzita, [2005], [cit. 2016-7-22]. Dostupný z WWW: http://www.svod.cz. Verze 7.0 [2007], ISSN 1802 – 8861.
- ↑ DAY, D. W. – JASS, J. R. – PRICE, A. B.. Morson and Dawson's Gastrointestinal Pathology,. 4. edition. Malden, Massachusetts, USA. : Blackwell Science Ltd, 2003. pp. 32-33. ISBN 9780470755983.
- ↑ GUNTURU, K. S. – WOO, Y. – BEAUBIER, N.. Gastric cancer and trastuzumab: first biologic therapy in gastric cancer. Therapeutic Advances in Medical Oncology. 2013, y. 2, vol. 5, p. 143-151, ISSN 1758-8340. DOI: 10.1177/1758834012469429.
References[edit | edit source]
- SMITH, Malcolm-G – HOLD, Georgina-L – TAHARA, Eiichi. Cellular and molecular aspects of gastric cancer. World J Gastroenterol [online]. 2006, vol. 12, no. 19, p. 2979-90, Available from <https://www.ncbi.nlm.nih.gov/pubmed/16718776>. ISSN 1007-9327.
- FOX, James G – WANG, Timothy C. Inflammation, atrophy, and gastric cancer. J Clin Invest [online]. 2007, vol. 117, no. 1, p. 60-9, Available from <https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1716216/?tool=pubmed>. ISSN 0021-9738.
- JAN ŽALOUDÍK Karcinom žaludku: DOPORUČENÉ POSTUPY PRO PRAKTICKÉ LÉKAŘE [online]. In: . Česká lékařská společnost Jana Evangelisty Purkyně, 2016 [cit. 2016-4-23]. Dostupné z: www.cls.cz/dokumenty2/os/r103.rtf
Recommended literature[edit | edit source]
- PETRUŽELKA, Luboš – KONOPÁSEK, Bohuslav. Klinická onkologie. 1. edition. Praha : Karolinum, 2003. 274 pp. ISBN 80-246-0395-0.
- KRŠKA, Zdeněk – HOSKOVEC, David. Chirurgická onkologie. 1. edition. Praha : Grada, 2014. 904 pp. ISBN 978-80-247-4284-7.
- KLENER, Pavel. Základy klinické onkologie. 1. edition. Praha : Galén, c2011. ISBN 9788072627165.