Cardiotonics
Cardiotonics (cardiostimulants) potentiate heart function by increasing heart rate (chronotropy) and myocardial contractility (inotropy), which increases cardiac output and arterial pressure. Many of them also have a positive dromotropic and lusitropic effect. Some of these drugs cause systemic vasodilation, while others have vasoconstrictive effects. The effects of these drugs on the heart muscle predispose them to use in heart failure, cardiogenic shock and hypotension[1]. In the treatment of heart failure, procedures that reduce the demands on myocardial function are preferred over cardiotonics- ie reduce afterload or preload, or both (diuretics, organic nitrates, calcium channel blockers, ACE inhibitors). [2]
Heart failure and cardiogenic shock[edit | edit source]
The main cause of heart failure and hypotension caused by acute heart failure (cardiogenic shock) is loss of myocardial contractility, which leads to reduced organ perfusion and hypotension. Cardiac function can be improved by reducing afterload, increasing preload (increased fluid volume) and increasing cardiac contraction. Cardiotonics work by this mechanism. Sympathomimetics or phosphodiesterase inhibitors are used for short-term therapy and may be harmful if used for a long time [1]. In contrast, cardiac glycosides (digitalis and others) are safe and effective in the long-term treatment of heart failure[1].
Circulatory shock[edit | edit source]
It is a form of shock caused by hypovolemia (for example in bleeding conditions) or vasodilation during infection (septic shock). Cardiotonics, especially sympathomimetics such as beta-agonists, are used to improve (ie increase) blood pressure. They are often used in conjunction with infusions and vasoconstrictor drugs.
General classes of drugs and their mechanisms of effect[edit | edit source]
Cardiotonics can be divided into four basic classes: beta-adrenoceptor agonists (beta-agonists), cardiac glycosides (digitalis and others), phosphodiesterase inhibitors and calcium sensitizers.
Beta-agonists[edit | edit source]
These are sympathomimetics that bind to cardiac β-adrenoreceptors. Activation of β-1 and β-2 adrenergic receptors leads to an increase in heart rate and contractility, which increases cardiac output. Their activation also has a positive dromo- and lusitropic effect. These drugs are indicated for both acute and refractory heart failure and circulatory shock. Β-Adrenoceptor agonists bind to β-receptors in the heart and smooth muscle. They also have effects in tissues other than the heart, especially in the smooth muscle of the bronchi (relaxation), liver (stimulating glycogenolysis) and kidney (stimulating renin release). They therefore cause cardiac pacing (increased heart rate, contractility, rate of transfer, relaxation) and systemic vasodilation. An increase in arterial pressure may occur, but not necessarily, as a decrease in vascular resistance interferes with an increase in cardiac output. Thus, the final effect on blood pressure depends on the relative effect on cardiac or vascular receptors [1]. β-agonists cause β-receptor down-regulation, which limits their use to short-term. As they are catecholamines (and have low bioavailability), they must be administered by intravenous infusion[1].
The principle of operation of β-adrenergic receptors - see above.
Specific drugs and their therapeutic use[edit | edit source]
The table shows several different β-agonists that are used clinically to treat heart failure and circulatory shock. These are either natural catecholamines or their analogues. Almost all have a certain degree of α-agonist activity. For some of these drugs, receptor selectivity is highly dose dependent.
| Medicine | Receptor selectivity | Clinical use | Comment |
|---|---|---|---|
| Adrenaline | β-1 = β-2> α-1 = α-2 | Anaphylactic shock; cardiogenic shock; cardiac arrest; | Low doses cause cardiac pacing and vasodilation. It has a vasoconstrictive effect at high doses. |
| Noradrenaline | β-1 = α-1 > β-2 = α-2 | Severe hypotension; septic shock | Reflex bradycardia masks the direct stimulatory effects on the SA node. |
| Dopamine | β-1 = β-2 > α-1 | Acute heart failure, cardiogenic shock and acute renal failure | Biosynthetic precursor of noradrenaline, stimulates its release.
At low doses, it stimulates the heart and reduces systemic vascular resistance. It has a vasodilating effect at high concentrations. |
| Dobutamine | β-1 > β-2 > α-1 | Biosynthetic precursor of noradrenaline, stimulates its release.
At low doses, it stimulates the heart and reduces systemic vascular resistance. It has a vasodilating effect at high concentrations. |
The effect is cardiac pacing with weak vasodilation. |
| Isoproterenol | β-1 = β-2 | Bradycardia and AV block. | The effect is cardiac pacing and vasodilation with little change in pressure. |
Side effects and contraindications[edit | edit source]
The main side effect of β-agonists is cardiac arrhythmias. Because they increase myocardial oxygen demand, they can accelerate the development of angina pectoris in patients with coronary artery disease. They can also cause headache and tremors[1].
Cardiac glycosides (digitalis)[edit | edit source]
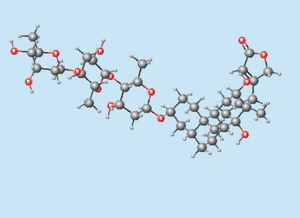
They have been used for more than 200 years to treat heart failure. They represent a family of compounds derived from the plant Digitalis purpurea (foxglove). These drugs inhibit Na + / K + ATPase in cardiac sarcolemma, leading to an increase in intracellular calcium through the Na + / Ca 2+ -exchange system. The increase in intracellular calcium subsequently stimulates the release of additional calcium from the sarcoplasmic reticulum, its binding to troponin C, which increases contractility.
Due to the long half-life of digitalis, this fact should be considered when dosing. It should be administered for several days to reach its therapeutic plasma level (0.5-1.5 ng / ml[1]).. Digitalis has a relatively narrow therapeutic window. Plasma concentrations higher than 2.0 ng / ml can be toxic [1]. Digitalis toxicity is manifested by (sometimes life-threatening) cardiac arrhythmias. Digibind (immune mechanism) or potassium supply are used to reduce digitalis levels (especially if toxicity is associated with hypokalemia).
Therapeutic use:
Heart failure[edit | edit source]
Digitalis compounds have cardiotonic effects and are used in heart failure. Although new and more effective drugs are already available, digitalis is still widely used. Clinical studies in patients with heart failure have shown that digoxin, when used in combination with diuretics and vasodilators, increases cardiac output and ejection fraction and reduces filling and capillary wedge pressures [1]. This reduces congestion in the lungs and the risk of edema. Heart rate changes slightly. These effects are expected with a drug that increases inotropy.
Atrial fibrillation a flutter[edit | edit source]
Atrial fibrillation a atrial flutter lead to an accelerated ventricular rate that can affect their filling (reducing their filling time). Digoxin and other drugs in this group are useful in reducing the ventricular rate, which was initiated by the increased rate of atrial contractions. The mechanism of this beneficial action of digoxin is its parasympathomimetic effect. Activation of the vagus can reduce the rate of conduction through the atrioventricular node to the point that some impulses are blocked. A smaller number of pulses is then fed to the chambers and the frequency of the chamber contractions decreases. In addition, digoxin increases the relative refractory period in the AV node.
Specific drugs from the group of glycosides[edit | edit source]
| Drug | Oral absorption | Half time (hours) | Elimination |
|---|---|---|---|
| Digoxin | 75 % | 40 | kidneys |
| Digitoxin | >90 % | 160 | liver |
| Oubain | 0 % | 20 | kidneys |
Note: Oubain is no longer used today. [2]
Side effects and contraindications[edit | edit source]
The most significant side effect of digitalis is cardiac arrhythmias, especially atrial tachycardia and atrioventricular block. The drug is contraindicated in patients with hypokalemia, AV block or Wolff-Parkinson-White syndrome. Impaired renal function leads to increased plasma concentrations of digitoxin as it is eliminated by the kidneys.
Phosphodiesterase inhibitors[edit | edit source]
These are drugs that inhibit the enzyme( cAMP-dependent phosphodiesterase, PDE) responsible for reducing cAMP. This leads to an increase in cAMP levels, which has a positive inotropic and chronotropic effect in the heart. cAMP is the second messenger in the pathway initiated by the binding of catecholamines to beta1-adrenergic receptors coupled to Gs-proteins. This is followed by activation of the adenyl cyclase and the formation of cAMP. cAMP (by reaction with other intracellular messengers) increases contractility, heart rate and conduction velocity.
These drugs are used to treat acute and refractory heart failure, but not chronic heart failure. The drugs used target cAMP-dependent phosphodiesterase (PDE3) isoform 3 [1].
Therapeutic indication[edit | edit source]
The pacing and vasodilatory properties of PDE3 inhibitors predispose them to the treatment of heart failure. Artery dilation reduces the afterload of a failing ventricle and leads to an increase in ejection fraction and organ perfusion. Reduction of afterload leads to a secondary decrease in preload, which increases the mechanical efficiency of the dilated heart and reduces the oxygen requirements of the failing myocardium. The pacing effect of these drugs increases inotropy, which leads to an increase in heart rate and ejection fraction. However, tachycardia is also the result, so drugs are dosed to minimize the positive chronotropic effect. Baroreceptor reflex,which occurs in response to hypotension, may also contribute to tachycardia. Clinical trials have shown that long-term therapy with PDE3 inhibitors increases the mortality of heart failure patients. These drugs are very useful in the treatment of acute decompensated heart failure[1]. They are always used together with other drugs such as diuretics, ACE inhibitors, β-blockers or digitalis.
Specific drugs[edit | edit source]
PDE3 inhibitors are milrinone a amrinone (possibly emoximone and piroximone[2]). (PDE5 inhibitors are used to treat erectile dysfunction).
Side effects and contraindications PDE3 inhibitors[edit | edit source]
The most common and at the same time most serious side effect of PDE3 inhibitors are ventricular arrhythmias, some of which can reach life-threatening proportions. Some patients may experience headaches and low blood pressure[1].
Calcium sensitizers[edit | edit source]
They represent the latest class of cardiostimulants. These drugs increase the sensitivity of troponin-C to calcium, so more calcium binds to it, which increases the contractility of the heart. These drugs are currently undergoing clinical trials for possible use in heart failure [1]. These include, for example, some phosphodiesterase III inhibitors (sulmazol, imobendan, levosimendal) [2].