Blood pressure regulation
Definition of blood pressure[edit | edit source]
blood pressure is the pressure exerted by the blood on the walls of the blood vessels and the heart. Mostly we mean blood pressure in the arteries of the systemic volume. We distinguish between systolic (100–140 mmHg) and diastolic (60–90 mmHg) pressures. 1 mmHg can then be expressed as 0.133 kPa.
Blood pressure can be explained by several equations:
P = T / r - pressure is directly proportional to the tension of the vessel wall and indirectly proportional to the radius of the vessel (Laplace's law).
P = Q × R - pressure is directly proportional to blood flow and vascular resistance.
we calculate by subtracting diastolic from systolic pressure. It's usually around 50 mmHg.
(MAP = mean arterial pressure) is then the pressure averaged over time: MAP = diastolic pressure + 1/3 of the pressure amplitude.
Thus, blood pressure can be affected by cardiac output per minute, total vascular resistance, central venous pressure, and blood volume.
Pressure changes during the heart revolution
Pressure changes during the heart revolution[edit | edit source]
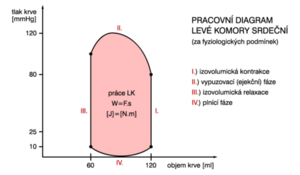
During the filling phase of the chamber (diastole), the volume of the chamber increases and the pressure increases by passively stretching the walls (but the pressure increase is small). At the end of diastole, there is a so-called end-diastolic pressure in the ventricle, which is less than 10 mmHg and is higher in the left ventricle (therefore it must have stronger muscle). At the MZ point, the atrioventricular valve closes as soon as the pressure in the ventricles exceeds the pressure in the atria. Then there is an isometric contraction, in which the pressure in the chambers increases without volume changes. At point AO, the semilunar valves open as soon as the pressure in the ventricles exceeds the pressure in the aorta and lungs. Furthermore, the ejection phase occurs, during which blood is expelled into the aorta and lungs. At point AZ, the semilunar valves close, and the pressure decreases at a constant volume.
Differences in the bloodstream[edit | edit source]
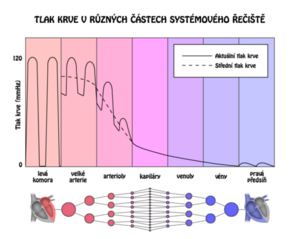
Small arteries and arterioles make up 50% of the total peripheral resistance, capillaries only about 25%. The veins have a very low pressure, which is why they serve as a reservoir in the blood, from which the blood is pumped into the whole organism if necessary.
Blood pressure regulation[edit | edit source]
2 concepts are important for pressure regulation:
vasoconstriction
In it, vasoconstrictors bind to the receptor and, through G-protein, induce an increase in intracellular Ca 2+. This depolarizes the membrane - the entry of Ca2 + L-type voltage-gated channels and at the same time the second messenger releases Ca2 + from the sarcoplasmic reticulum. This causes the smooth muscle to contract in the blood vessel wall (greater contraction force). Examples of vasoconstrictors are endothelin 1, thromboxane A2, angiotensin II, noradrenaline (sympathetic).
vasodilation
It removes Ca2 +, which goes out of the cell through Ca2 + -ATPase = PMCA and Ca2 + - Na shift and also back to the ER (Ca2 + ATPase = SERCA). Vasodilators increase the levels of guanosine monophosphate (cGMP) or adenosine monophosphate (cAMP), which stimulate SERCA and PMCA via protein kinases, so that the intracellular Ca 2+ content decreases and in addition the voltage-gated Ca 2+ channel (verapamil and dihydropyridine) is inhibited. Vasodilators include nitric oxide and prostacyclin.
Acute blood pressure regulation - baroreceptor reflex
The high-pressure baroreceptors are in the aorta and carotid sinus.
This system works in such a way that the pressure drop reduces the artery wall tension and reduces the activity of the barorecetors. This increases the activity of the sympathetic nerves, which increases the heart rate and contractility, peripheral vasoconstriction and venoconstriction (eg when the body is erect). This process will increase the pressure again.
Long-term blood pressure regulation[edit | edit source]
The amount of fluid excreted by the kidneys[edit | edit source]
If the pressure increases, the filtration pressure in the kidneys increases. This will increase the volume of urine, which will reduce the volume of extracellular fluid, ie blood. This reduces cardiac output.
antidiuretic hormone
Vasoconstriction increases the resorption of water in the glomeruli, which increases blood volume and increases venous return.
Aldosterone
It is produced by the adrenal cortex. Increases the resorption of Na + and water. This will increase blood volume and venous return. Thus, cardiac output is increased and, in addition, sensitivity to angiotensin II increases, thus increasing the efficacy of the renin-angiotensin system.
systemic renin-angiotensin
Renin is secreted by the kidney when blood flow decreases (sympathetic effect). It cleaves the decapeptide angiotensin I from alpha 2 globulin, which has no significant activity but is converted in the lungs by angiotensin converting enzyme to angiotensin II.
Angiotensin II has two main functions:
- vasoconstriction arterioles,
- water retention and Na + - shift of the functional renal curve.
Thus, the renin-angiotensin system increases blood volume (hence minute output) as well as peripheral resistance.
Local blood pressure control
Local blood pressure control is the ability of tissues to independently regulate blood flow.
Autoregulation
Autoregulation is the ability to maintain a constant flow in the pressure range of 50-170 mmHg through a myogenic response. Arteriol constriction occurs in response to vascular wall tension (activation of tensile-activated Ca 2+ channels) through locally generated vasodilatory factors (increased flow dilutes them, resulting in vasoconstriction).
Metabolic factors
The response to hyperemia (increased blood flow) caused by K +, CO2 and adenosine is vasodilation.
Local hormones
During inflammation, histamine and bradykinin are released, which cause vasodilation and increase vascular permeability. As a result, swelling occurs. Leukocytes and antibodies penetrate the damaged tissues, increasing the activity of NO (vasodilator) production.
Links[edit | edit source]
[edit | edit source]
References
- WARD, P.T. Jeremy a W.A. Roger LINDEN. Základy fyziologie. 1. vydání. 2010. ISBN 978-80-7262-667-0.
- TROJAN, Stanislav, et al. Lékařská fyziologie. 4. vydání. Praha : Grada, 2004. 772 s. ISBN 80-247-0512-5.
- BRAVENÝ, Pavel. Poznámky k přednáškám z fyziologie : Srdce a krevní oběh; Dýchání; Ledviny; Acidobazická rovnováha; Svaly. 1. vydání. 1993. ISBN 80-85467-60-7.
- GANONG, William F. Přehled lékařské fyziologie. 20. vydání. Galén, 2005. 890 s. ISBN 80-7262-311-7.
- SILBERNAGL, Stefan a Despopoulos AGAMEMNON. Atlas fyziologie člověka. 6. vydání. 2004. ISBN 80-247-0630-X.