Vitamine D
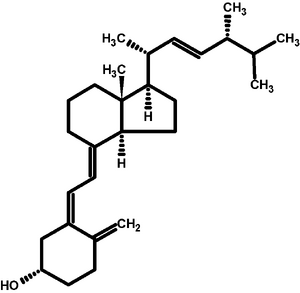
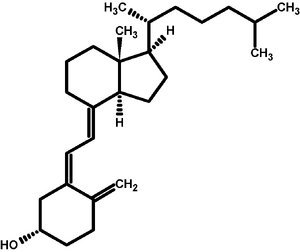
Vitamin D is a group of substances (calciferols) that belong to the fat-soluble vitamins and play an irreplaceable role in calcium phosphate metabolism , as they are necessary for proper bone mineralization . It was first identified as a substance in yeast and classified as a vitamin.[1] Since it is converted (double hydroxylation) into an active metabolite in the body, it can be called a hormone. Thus, according to recent findings, vitamin D is a pleiomorphic steroid hormone that plays a fundamental role in the development and maintenance of bone tissue, muscles, immunity, regulation and protection against heart and oncological diseases. [2]
Ergocalciferol (D2) is of vegetable origin and cholecalciferol (D3) of animal origin. The main source of vitamin D3 is endogenous production in the skin, where it is produced from the provitamin 7-dehydrocholesterol under the action of UVB ultraviolet radiation . To a lesser extent, the source of vitamin D is plant and animal food or foods supplemented with vitamin D. Due to the insufficient intake of vitamin D through natural food, many countries (outside the Czech Republic) fortify selected foods (milk, butter, margarines, yogurts, some cereals) with the addition of vitamin D2 or D3.[1]
Vitamin D2 or D3 (endogenous or from the diet) is hydroxylated twice in the body, first in the liver and then in the kidneys, to form calcitriol - an active metabolite of vitamin D. It is transported in the blood bound to vitamin D-binding protein (DBP) formed in the liver . Calcitriol then acts via the intracellular vitamin D receptor (VDR). It has a short metabolic half-life (approx. 4 hours).
Importance of vitamin D
- maintenance of calcium and phosphorus homeostasis by direct effect on intestine, kidney and bone:
- increases calcium absorption in the small intestine and kidney tubules by actively acting on calcium channels;
- regulates osteoblast differentiation ;
- stimulates the expression of alkaline phosphatase in the bone matrix;
- stimulates the formation of osteoclasts (osteoclastogenesis) through cellular interaction with osteoblasts and cellular precursors of osteoclasts;
- promotes bone mineralization;
- inhibits parathyroid hormone , which induces bone resorption; [2]
- it also has a number of extraskeletal effects – receptors for vitamin D (VDR) are present in most tissues of the human body and at the same time a number of (extra-renal) cells and tissues are able to hydroxylate 25-OHD to calcitriol, however, many extraskeletal effects of vitamin D have not yet been detailed clarified;
- the presence of VDR in macrophages , dendritic cells , T and B lymphocytes supports the assumption of the importance of vitamin D for the immune system;[3] experimental studies have shown that a complete deficiency of vitamin D leads to severe immunopathologies; [4] a reduced level of vitamin D is associated with a higher incidence of viral infections of the upper respiratory tract;[5][6][7]
- calcitriol acts on muscle cell receptors and at low concentrations (below 30 nmol/l) muscle strength decreases significantly and the risk of falls increases in older women and men;[8]
The daily requirement here varies between 200-2000 IU, this value should not be exceeded according to the recommendation. The need for vitamin D is significantly increased during pregnancy. An overdose of vitamin D is very rare and practically always caused by the artificial administration of drugs, varying in values of daily intake of 5,000-10,000 IU. In an inappropriate combination with the diet, it can already be a value of around 4,000 IU, when the clinical and laboratory picture is dominated by significantly increased calcium in the blood and urine.[2] Excessive supplementation of vitamin D can lead to the development hypercalcemia, nephrocalcinosis and formation kidney stones.[3]
A deficiency of vitamin D is then manifested by a mineralization disorder, i.e. rickets in a growing organism, respectively osteomalacia in adults. A smaller degree of vitamin D deficiency leads to reduced absorption of calcium with a subsequent decrease in the concentration of calcium in the circulation (mainly ionized) and a subsequent rise in the concentration of parathyroid hormone (secondary hyperparathyroidism). An increased concentration of parathyroid hormone in the circulation intensifies the activity of 1-α hydroxylase with a subsequent rise in the active form of vitamin D and simultaneously stimulates bone resorption. During childhood and adolescence, even a subclinical lack of vitamin D has negative consequences, as it prevents the full development of the skeleton (i.e. reaching peak bone mass) and the consequence is a more frequent occurrence of fractures and osteoporosis. [1]
Breast milk has a low vitamin D content, therefore supplementation with vitamin D3 is recommended for newborns , which is not only better absorbed, but also has better pharmacokinetic and pharmacodynamic properties than vitamin D2. It seems that vitamin D could also influence the immune function of the newborn. [1][9]
Source and metabolism[edit | edit source]
The main source of vitamin D3 is endogenous production in the skin , where it is produced from 7-dehydrocholesterol (provitamin) under the action of UVB ultraviolet radiation (with a wavelength of 290–315 nm ). The amount of vitamin D3 synthesized in the skin depends on the availability of 7-dehydrocholesterol and on exposure to UV radiation (season, latitude, air pollution, use of sunscreen, covering the body). Melanin competes with 7-dehydrocholesterol in the skin for photons of UV radiation, which therefore reduces the production of vitamin D3. Therefore, people with dark skin need longer exposure to sunlight to create adequate amounts of vitamin D. In areas above 40 degrees north and below 40 degrees south latitude in the winter months, the sun moves above the horizon at such an unfavorable angle that vitamin D is practically not produced in the skin. With long-term sun exposure, vitamin D intoxication does not occur due to the photolytic conversion of provitamin D3 into tachysterol and lumisterol, which are inactive metabolites. [4][10]
Vitamin D can also be obtained to a lesser extent from the diet . Vitamin D3 is contained in fish liver oil, fatty fish or egg yolk. Vitamin D2 can be synthesized by plants and fungi by the action of UVB on ergosterol (a provitamin). Vitamin D is absorbed from the diet in the small intestine (in the duodenum and jejunum) in the form of chylomicrons, which enter the bloodstream via the lymphatic system via the superior vena cava. [3]
Both D2 and D3 are biologically inactive and are activated in two steps (two-step hydroxylation): in the liver they are changed (by the enzyme 25-hydroxylase) to biologically inactive 25-hydroxycholecalciferol (25-OHD, calcidiol, calcifediol), which is further changed mainly in the kidneys but to a lesser extent also in other tissues (by the enzyme 1α-hydroxylase) to the active form of vitamin D 1,25-dihydroxycholecalciferol (1,25(OH) 2 D, calcitriol ). The main regulatory factors of hydroxylation are the level of parathyroid hormone, phosphorus and calcium. This active reconstruction that makes the vitamin de factohormone, takes place mainly in the kidneys, but many other tissues have the necessary enzyme equipment, which can "locally produce" active vitamin D for the needs of their own metabolic processes. [1] Local production of calcitriol occurs, for example, inside macrophages, lymphocytes, placenta, keratinocytes, hair follicles, pancreas, endothelium, adrenal glands, colon, prostate, brain, mammary glands. [10] Calcidiol and calcitriol circulate in the blood mainly bound to vitamin D binding protein (DBP). Calcitriol triggers metabolic processes through the intracellular vitamin D receptor (VDR).
| Vitamin D | Parathyroid hormone | Calcitonin | |
|---|---|---|---|
| kidneys | ↑ reabsorption Ca2+ and phosphates | ↑ reabsorption Ca2+ and excretion of phosphates, stimulates the production of calcitriol |
↑ excretion of Ca2+, ↑ excretion of phosphates |
| bone | bone mineralization; high levels, on the other hand, decalcify |
bone resorption (osteoclast activation), calcemia and phosphatemia rise |
inhibition of osteoclasts, deposition of Ca2+ in bones |
| intestine | stimulates resorption of Ca 2+ and phosphates | stimulates the production of calcitriol → stimulates the resorption of Ca2+ and phosphates |
– |
Conversion of vitamin D3 units in sources: 1 µg = 40 IU .
Daily recommended dose: According to DACH 2000[13] , from 1 to 65 years is 5 µg, over 65 years is 10 µg. A new revision of the American recommended doses (IOM 2011) assumes a minimum exposure to sunlight (recommended prevention of skin malignancies by sun protection) recommends 15 µg from 1 to 70 years, 20 µg over 70 years .[14].
The daily loss of calcium from the body is about 200 mg (mainly through urine and the skin surface) and this must be supplemented daily with a balanced metabolism. If the transport in the intestinal wall were completely passive, the daily intake of calcium would have to be at least 2,500 mg in order to (passively) absorb the necessary 200 mg. With active transport, ensured primarily by sufficient vitamin D, approx. 16% of the received dose is absorbed, which means that to replace the 200 mg loss, the daily intake of calcium through food must be at least 1,000–1,200 mg. [1]
Determination[edit | edit source]
Saturation of the body with vitamin D is evaluated using the serum concentration of 25-OHD , which has a relatively long half-life (2 to 3 weeks).[4]
Determination of the active form of vitamin D (1,25(OH) 2 D) is performed only in case of nephropathy, otherwise it is not recommended due to its short half-life (4 to 7 hours) and because its serum concentration is significantly influenced by, for example, parathyroid hormone . [4]
The gold standard is the LC-MS/MS ( Liquid chromatography-mass spectrometry ) method, but immunochemical methods are more commonly used due to its economic, equipment and personnel demands . [4]
Conversion of 25-OHD units in plasma: 2.5 nmol/l = 1 ng/ml
Deficit[edit | edit source]
A serum 25-OHD concentration <50 nmol/l is most commonly defined as vitamin D deficiency, but there is no unequivocal agreement regarding this value. This value was determined based on the analysis of the effect of 25-OHD on markers of bone metabolism, especially in relation to parathyroid hormone (PTH). (Clinically significant vitamin D deficiency leads to PTH elevation after some time.) [4]
Normal plasma values of Ca, P, alkaline phosphatase (ALP) and parathyroid hormone also indicate an adequate supply of vitamin D. In the case of vitamin D deficiency, little calcium is absorbed, PTH is secreted → osteoclasts are activated → ALP in the serum rises. Increased values of parathyroid hormone (secondary parathyroidism) appear at a 25OH D concentration of 10–25 nmol/l, with insufficient calcium intake up to 50 nmol/l[13]
With a lack of vitamin D, the deposition of calcium in the newly formed bone is disturbed and the bones become deformed. Clinical manifestations of vitamin D deficiency are rickets in children (deformities of the long bones of the lower limbs, craniotabes, caput quadratum, Harrison's groove) and osteomalacia in adults (mainly deformities of the long bones of the lower limbs and pelvic bones). Vitamin D deficiency in later life also contributes to osteoporosis . Unlike osteomalacia, in osteoporosis the normally mineralized bone mass is reduced, the bones are brittle and break easily, but do not deform. Can be differentiated on x-ray.
Clinical manifestations of vitamin D deficiency occur on all continents, the risk group is especially children under 30 months, mostly infants - there is little vitamin D in mother's milk, they are not exposed to much sunlight and their growth is very intense (great need).
In recent years, subclinical deficiency (low level of 25OHD) has been described in a significant percentage of the population both in North America and in Europe, but the IOM [14] points out the lack of a general consensus on the adequate level of plasmatic 25OHD, and thus there is a possibility of overestimating the prevalence of deficiency in the population.
Prevention: In the Czech Republic, the administration of vitamin D is recommended from 2 weeks during the entire first year and in the winter months of the second year of life.
Excess[edit | edit source]
Hypervitaminosis occurs with an overdose of food supplements. It leads to hypercalcemia and eventually to soft tissue calcification - damage to the heart and kidneys.
Most often, hypervitaminosis occurs in infants during improper prevention of rickets. Symptoms appear after 1-3 months of administration of excessive amounts of vitamin D: hypotonia, anorexia, irritability, polyuria, polydipsia → dehydration, constipation, palpable skyballs in the abdomen, thirst, pallor, vomiting.
The upper limit of daily long-term tolerable intake of vitamin D for adults is 50 μg according to DACH 2000 and 100 μg according to IOM [14].
Note[edit | edit source]
From an evolutionary point of view, vitamin D is one of the oldest hormones, which is also produced by some of the first forms of life - phytoplankton. [3]
In recent years, considerable attention has been paid to the possible additional roles of vitamin D in the human body. Vitamin D receptors (VDR) are present practically everywhere in the body, even in tissues that are not related to calcium and phosphorus homeostasis, and genetic studies show that calcitriol affects the transcription of several hundred genes - 5% of the human genome . On this basis, some experts hypothesize a potential preventive and therapeutic role of vitamin D in connection with a whole range of diseases (tumor and autoimmune diseases including type 1 diabetes, type 2 diabetes, cardiovascular diseases, hypertension, infectious diseases, neuropsychiatric disorders and preeclampsia).
However, the American Institute of Medicine (IOM) [14]in 2011, after an exhaustive analysis, stated that the current evidence on the extraskeletal role of vitamin D is inconsistent and inconclusive.
Links[edit | edit source]
Related articles[edit | edit source]
- Vitamins • Fat Soluble Vitamins • Vitamins in diet
- Calcium phosphate metabolism • Disorders of Calcium And Phosphate Metabolism
References[edit | edit source]
- ↑ a b c d e f PALIČKA, V. Vitamin D:skeletal and extraskeletal effect. Med. praxi [online]. 2013, vol. 5, p. 199–202, Available from <https://www.medicinapropraxi.cz/pdfs/med/2013/05/07.pdf>.
- ↑ a b c NOVOSAD, P. Calcium and vitamin D in the primary and secondary prevention of osteoporosis. Med. practice [online]. 2017, vol. 5, p. 217–223, Available from <https://www.praktickelekaranstvi.cz/pdfs/lek/2018/89/02.pdf>.
- ↑ a b c d PLUDOWSKI, Pawel – HOLICK, Michael F. – GRANT, William B.. Vitamin D supplementation guidelines. The Journal of Steroid Biochemistry and Molecular Biology. 2018, vol. 175, p. 125-135, ISSN 0960-0760. DOI: 10.1016/j.jsbmb.2017.01.021.
- ↑ a b c d e f MARATOVÁ, K. , et al. Vitamin D and its supplementation in pediatric patients with inflammatory bowel disease. Pediatrics for practice [online]. 2018, y. 19, vol. 4, p. 190-194, Available from <www.pediatriepropraxi.cz>. ISSN 1213-0494.
- ↑ SABETTA, James R – DEPETRILLO, Paolo – CIPRIANI, Ralph J. , et al. Serum 25-hydroxyvitamin d and the incidence of acute viral respiratory tract infections in healthy adults. PLoS ONE [online]. 2010, vol. 5, no. 6, p. 11088, Available from <https://doi.org/10.1371/journal.pone.0011088>. ISSN 1932-6203.
- ↑ BERGMAN, Peter – NORLIN, Anna-Carin – HANSEN, Susanne. , et al. Vitamin D3 supplementation in patients with frequent respiratory tract infections: a randomised and double-blind intervention study. BMJ Open [online]. 2012, vol. 2, no. 6, p. 1140, Available from <https://doi.org/10.1136/bmjopen-2012-001663>. ISSN 2044-6055.
- ↑ NORLIN, Anna-Carin – HANSEN, Susanne – WAHREN-BORGSTRÖM, Emilie. , et al. Vitamin D3 Supplementation and Antibiotic Consumption - Results from a Prospective, Observational Study at an Immune-Deficiency Unit in Sweden. PLoS ONE [online]. 2016, vol. 11, no. 9, p. e0163451, Available from <https://doi.org/10.1371/journal.pone.0163451>. ISSN 1932-6203.
- ↑ HRDÝ, P – NOVOSAD, P. New insights into vitamin D function. Practice pharmacies [online]. 2015, y. 11, vol. 2, p. 52-54, Available from <https://www.praktickelekarenstvi.cz/pdfs/lek/2015/02/03.pdf>.
- ↑ WALKER, Valencia P – ZHANG, Xiaoran – RASTEGAR, Ida. Cord blood vitamin D status impacts innate immune responses. J Clin Endocrinol Metab [online]. 2011, vol. 96, no. 6, p. 1835-43, Available from <https://doi.org/10.1210/jc.2010-1559>. ISSN 0021-972X (print), 1945-7197.
- ↑ a b BAYER, M. Fat soluble vitamins. Practical pharmacy [online]. 2008, y. 4, vol. 5, p. 235-237, Available from <https://www.solen.cz/pdfs/lek/2008/05/10.pdf>.
- ↑ SILBERNAGL, Stefan – DESPOPOULOS, Agamemnon. Atlas of Human Physiology : 6. edition, completely revised and expanded. 3. edition. Prague : Grada, 2004. pp. 290-293. ISBN 80-247-0630-X.
- ↑ LEBL, J – JANDA, J – POHUNEK, P, et al. Clinical pediatrics. 1. edition. Galén, 2012. 698 pp. pp. 189-196. ISBN 978-80-7262-772-1.
- ↑ a b Deutsche Gesellschaft für Ernährung, Österreichische Gesellschaft für Ernährung, Sweizerische Gesellschaft für Ernährungforschung, Sweizerische Vereinigung für Ernährung. . Referenzwerte für die Nährstoffzufuhr (DACH). 1. edition. Frankfurt am Main : Umschau/Braus, 2000. 216 pp. ISBN 3-8295-7114-3.
- ↑ a b c d ROSS, AC. Dietary Reference Intakes for Calcium and Vitamin D. 1. edition. Washington D.C : Institute of Medicine (IOM); National Academy of Sciences, 2011. 1132 pp. ISBN 978-0-309-16394-1.