Calcium phosphate metabolism
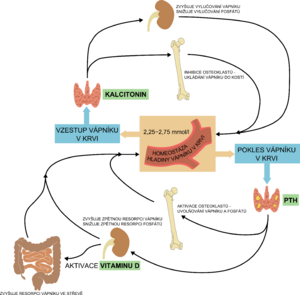
Calcium phosphate metabolism or calcium and phosphorus management is hormonally regulated by parathyroid hormone , calcitonin and vitamin D.
Calcium[edit | edit source]
See the Calcium page for more information .
Calcium is one of the most important extracellular ions. It mediates the effect of hormones, humoral substances, cytokines and other mediators on cell metabolism. Calcium creates the structure of bones and teeth, participates in the regulation of neuromuscular activity, coagulation , heart activity. In the body, calcium makes up about 1.5% of the total body weight, with more than 99% of it in the bone. Calcium is found in milk, cheese, eggs and "hard water". The necessary amount of calcium is absorbed from the food in the intestine and the rest is excreted in the faeces and urine.
The importance of calcium[edit | edit source]
Significance of calcium and physiological functions related to the presence of calcium: inorganic component of bones and teeth , blood clotting factor (factor IV), kinin production , enzyme regulation, hormone release and their effect, regulation of tissue excitation, regulation of transmitter release, activates troponin in skeletal muscle , the formation of tropomyosin , thereby activating actin , activates contraction in smooth muscle by binding to calmodulin . Intracellularly, calcium contributes to the action potential of the cell, to contraction, to motility, to cell division, to the structural integrity of the cell, to increase glycolysis. A decrease in extracellular calcium concentration increases neuromuscular excitability and thus also the possibility of tetany .
Calcium resorption[edit | edit source]
The recommended daily dose for adults is about 1 g. Its resorption is physiologically around 25-40%. Calcium is resorbed actively in the duodenum and jejunum, passively in the ileum and colon. Calcium resorption takes place simultaneously with its secretion. Alkaline pH significantly reduces calcium resorption.
At the enterocyte level, calcium resorption occurs in two ways:
- Transcellular - On the side facing the intestinal lumen, the specific transport protein calbindin is used. On the basolateral membrane side, calcium is then actively transported in the presence of energy against the concentration gradient into the blood.
- Paracellular - Calcium is transported from the intestinal lumen directly, and calcium is transported to the paracellular space by release from the lysosome of the enterocyte.
Calcemia[edit | edit source]
The concentration of total calcium in serum (calcium) is 2.25-2.75 mmol / l, ionized serum calcium 1.1-1.4 mmol / l.
Calcium is in the blood in three forms:
- 50% in ionized form (most biologically active, able to diffuse across biological membranes, crucial for neuromuscular stimulation);
- 40% protein bound (not freely diffusible);
- 10-13% in the form of complexes (such as bicarbonate, phosphate, citrate).
Alkalosis in the blood leads to increased calcium binding to plasma proteins, thereby reducing free, ionized calcium, but the total calcium concentration does not change.
The binding of calcium to proteins depends on the pH of the blood - as the pH (alkalosis) increases, more binding sites for Ca 2+ are released on the proteins , and therefore ionized Ca 2+ decreases . Therefore, for example, tetany occurs as a result of hyperventilation . Hypoalbuminemia is associated with calcium depletion, but there are no symptoms of hypocalcemia because the ionized form is normal.
Phosphate metabolism is closely related to calcium metabolism. Intravenous administration of phosphates reduces serum Ca 2+ levels because calcium phosphate is formed and is deposited in the bones. In contrast, hypophosphataemia causes hypercalcemia by releasing Ca 2+ from the bones.
Calcium excretion[edit | edit source]
Only ionized calcium can be filtered by the kidneys. In the area of the proximal canal, resorption takes place both transcellularly (15–20%, active) and paracellularly (80–85%, passively). The ascending part of the Henle loop again absorbs calcium transcellularly and paracellularly.
Both parathyroid hormone and calcitonin stimulate reuptake by the transcellular pathway in this area of the nephron. Parathyroid hormone decreases the final concentration of calcium in the urine and calcitonin increases it. In the distal part of the nephron, in addition to parathyroid hormone, calcitonin and calcitriol, calcium resorption is involved.
Maintenance of calcium homeostasis[edit | edit source]
Calcium homeostasis is maintained by the activity of osteoclasts , which resorb bone, thus increasing serum calcium and the concomitant activity of osteoblasts , which are involved in bone formation, thereby reducing serum calcium. Hormones that maintain calcium homeostasis include calcitonin, parathyroid hormone and vitamin D with the involvement of the intestine, kidneys and bones. Regular and adequate physical activity of the body is also important for maintaining calcium homeostasis, which improves the absorption of calcium from the intestine by increasing blood flow to the splanchnic area and the formation and maintenance of bone mass. Calcium entry into cells can be reduced pharmacologically by calcium channel blockers . Calcium is a calcium antagonist.
Phosphates[edit | edit source]
See the Phosphate page for more information .
Reference limits :
- serum 0.7-1.5 mmol / l,
- urine 15-90 mmol / l,
- 80% of phosphates are stored in bones and teeth.
Regulation of calcium-phosphate metabolism[edit | edit source]
Calcium phosphate metabolism affects parathyroid hormone, calcitonin and vitamin D:
- parathyroid hormone (PTH) is a parathyroid peptide hormone; in hypocalcemia, the release of PTH into the blood increases;
- calcitonin (thyrocalcitonin, CT) is a peptide hormone produced by parafollicular (C-cells) of the thyroid gland; CT levels increase in hypercalcemia;
- Vitamin D (calcitriol, 1,25- (OH) 2 -cholecalciferol) is a lipophilic hormone produced in the skin by the action of UV radiation, further converted in the liver and completed in the kidneys.
Influence of individual hormones on calcium and phsphatemia:
- parathyroid hormone (PTH):
- bone: releases calcium (Ca) + phosphorus (P);
- kidney: increases reuptake Ca, decreases reuptake P;
- intestine - no direct effect (PTH increases the production of calcitriol in the kidneys and thus acts indirectly in the intestine).
- calcitonin
- bone: retains Ca + P;
- kidney: reduces reuptake of Ca + P;
- intestine - no direct effect (calcitonin probably reduces the production of calcitriol in the kidneys).
- vitamin D (calcitriol, 1,25- (OH) 2 -cholecalciferol)
| Parathyroid hormone | Calcitonin | Vitamin D[3] | |
|---|---|---|---|
| bone | osteoclast activation,
calcium and phosphatemia are increasing |
osteoclast inhibition,
Ca 2+ storage in bones |
skeletal mineralization;
high levels, on the other hand, decalcify |
| Kidneys | stimulates Ca 2+ resorption, inhibits phosphate resorption,
stimulates vitamin D synthesis |
increases Ca 2+ excretion ,
increases phosphate excretion |
increases the reabsorption of Ca 2+ and phosphates |
| Intestines | stimulates the resorption of Ca 2+ and phosphates | – | stimulates the resorption of Ca 2+ and phosphates |
Links[edit | edit source]
[edit | edit source]
- Disorders of calcium-phosphate metabolism • Indicators of bone remodeling, markers of bone resorption
- Osteoporosis • Osteomalacia • Rachitis • Hypoparathyroidism
Reference[edit | edit source]
- HAVRÁNEK, J .: Dysbalance of other ions.
- ↑Jump up to:a b c d e f g h i j WILHELM, Z. What is good to know about calcium. Practical pharmacy [online] . 2007, vol. -, vol. 4, pp. 184-189, also available from < http://solen.cz/pdfs/lek/2007/04/09.pdf >.
- ↑Jump up to:a b c d e SILBERNAGL, Stefan and Agamemnon DESPOPOULOS. Atlas of Human Physiology: 6th edition, completely reworked and expanded. 3rd edition. Prague: Grada, 2004. pp. 290-293. ISBN 80-247-0630-X .
- ↑ BENEŠ, Jiří. Study materials [online]. © 2007. [feeling. 2010]. < http://jirben.wz.cz >.
- ↑ GANONG, William F. Overview of Medical Physiology. 20th edition. Prague: Galén, 2005. 890 pp. 396. ISBN 80-7262-311-7 .