Vitamin A (biochemistry)
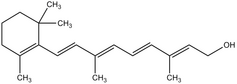
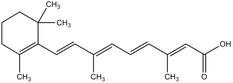
Vitamin A' includes retinol, retinal and retinoic acid. It is formed in the body from β-carotene and some other carotenoids. Bile secretion is required for resorption. Carotene is transported to the liver where it is metabolized to vitamin A and stored in stores. Zinc is required to mobilize vitamin A. In the blood, it is transported to RBG (retinol binding globulin). This is reduced in retinitis pigmentosa, proteinuria and low protein diet.
Vitamin A is required for membrane stabilization, epithelial maturation and differentiation, skin and mucosal integrity, keratinization, support of immune reactions, mucus production, bone and tooth metabolism, placenta development, spermatogenesis, and is an important precursor of rhodopsin. Deficiency or excess leads to rupture of lysosomal membranes and release of hydrolases.
Beta carotene, in addition to being a precursor of vitamin A, has antioxidant and antitumorigenic effects (it is involved in the prevention of the promoter phase of the carcinogenic mechanism, reducing the risk of lung cancer).
Source[edit | edit source]
Vitamin A as such is only in animal foods. The richest source is liver, with relatively little in egg yolks, fats and meat. Sources of beta carotene are green, red or orange vegetables and fruits.
Daily Recommended Adult Intake' according to DACH 2000[1] is 1 mg of retinol equivalents. Pregnant and lactating women have a higher need.
Beta carotene to retinol equivalents conversion ratio: Previously, the beta carotene to retinol equivalents conversion ratio was 6:1. Based on studies on the amount of carotenes needed to prevent night blindness if carotenes are the main source of vitamin A, the U.S. IOM changed this ratio to 12:1. [2]
That is:
- in the food composition tables, which are based on the original 6:1 conversion, the vitamin A content of foods is overestimated;
- vitamin A intake in populations is lower than expected.
Deficit[edit | edit source]
Food deficiency is rare in Europe with normal dietary habits, and can arise from fat resorption disorders (e.g. celiac disease, pancreatic disorders).
Globally, vitamin A deficiency ranks among the most important malnutrition diseases: it is the most common cause of childhood blindness in developing countries and contributes to the death of a significant number of children from common infections because even subclinical deficiency reduces immunity.[3]
Clinical manifestations'
- Affection of the eye - xerophthalmia: First appears scheroslepost (hemeralopia, wolf darkness), reversible xerosis conjunctivae (conjunctivae dry and thicken), silvery triangle-shaped Bitot spots. Irreversible changes may follow: softening of the cornea (keratomalacia) and ulceration healing by scarring.
- Immunodeficiency' - reduced resistance to infection.
- Changes of epithelium of various organs' - keratinizing metaplasia, dry scaly skin, follicular hyperkeratosis (Morbus Darier - skin involvement of face, neck, buttocks and extensors - pattern of sprinkled flour), metaplasia of laryngeal epithelium - hoarseness; lower respiratory tract - epithelium dries and peels → may obstruct bronchioles; metaplasia of urinary tract epithelium predisposes to pyuria and haematuria; vaginal mucosa also dry; hair lustreless.
- Other changes have also been described, but because the affected patients usually have other co-morbidities, the exact role of vitamin A is not clear.[4]
For assessing the status of population supply of vitamin A, the assessment of the prevalence of night blindness' and, more recently, plasma retinol levels' <0.70 μmol/l are used.[3]
Excess[edit | edit source]
Manifestations of hypervitaminosis occur only after preformed vitamin A. Retinoic acid is teratogenic. Pregnant women should therefore not consume liver (the richest source of vitamin A) during the first trimester of pregnancy, which may contain very high levels of retinol.[1]
A dangerous source of overdose can be ointments with retinoids (for psoriasis, etc.). Mothers treated with ointments may give birth to damaged children even 2 years after the end of treatment (Author not given!).
Acute hypervitaminosis is manifested by intracranial hypertension' - vomiting, somnolence, bulging of the large fontanelle and/or picture as in intracranial tumor (pseudotumor cerebri) - edema of the papilla, paralysis of the cranial nerves. It occurs after a dose in an adult >100x in a child >20x the recommended dose (dietary supplement, polar bear or shark liver).
Chronic hypervitaminosis' - appetite, nausea, vomiting, weight loss, diarrhea, alopecia, bleeding, bone fragility, hepatotoxicity (hepatomegaly and other signs of liver disorder). It occurs after weeks to years of consuming >10 times the recommended dose.
The upper limit of the daily long-term safe intake for adults is 3[1] mg of vitamin A, according to the DACH 2000[1].
Administration of high doses (up to 10 mg) of beta carotene' appeared to be harmless in large epidemiological studies, but in other studies, smokers after doses of 20 - 30 mg experienced an increase in lung cancer incidence.
Karotenemie[edit | edit source]
Long-term excessive consumption of carrots or other fruits or vegetables rich in carotene results in yellow skin discoloration - carotenemia - a benign condition because the conversion of carotene to vitamin A is slow. It differs from icterus in that the sclerae and mucous membranes are not yellow. Hypothyroidism, diabetes mellitus, liver and kidney disease may be associated with carotenemia due to impaired conversion of beta carotene - but it is not an excess from food.[5]
Links[edit | edit source]
Related articles[edit | edit source]
External links[edit | edit source]
Sources[edit | edit source]
- KARTHIK, SV. Carotenemia in infancy and its association with prevalent feeding practices. Pediatr Dermatol. 2006, y. 23, no. 6, p. 571-3, ISSN 0736-8046.
- BENEŠ, Jiří. Studijní materiály [online]. [cit. 2010]. <http://jirben.wz.cz>.
- BENCKO, Vladimír, et al. Hygiena. 2. edition. 2002. ISBN 80-7184-551-5.
References[edit | edit source]
- ↑ a b c d Deutsche Gesellschaft für Ernährung, Österreichische Gesellschaft für Ernährung, Sweizerische Gesellschaft für Ernährungforschung, Sweizerische Vereinigung für Ernährung. . Referenzwerte für die Nährstoffzufuhr (DACH). 1. edition. Frankfurt am Main : Umschau/Braus, 2000. 216 pp. ISBN 3-8295-7114-3.
- ↑ {Cite | type = book | isbn = 978-0309072908 | surname1 = Panel on Micronutrients | surname2 = Subcommittees on Upper Reference Levels of Nutrients and on Interpretation and Use of Dietary Reference Intakes | surname3 = Standing Committee on the Scientific Evaluation of Dietary Reference Intakes | Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc | edition = 1 | location = Washington D.C | publisher = National Academic Press | year = 2002 | range = 800 }}
- ↑ a b World Health Organization. . Global prevalence of vitamin A deficiency in populations at risk 1995-2005 : WHO Global Database on Vitamin A Deficiency [online] . 1. edition. Geneva : World Health Organization, 2009. 55 pp. Available from <http://apps.who.int/iris/bitstream/10665/44110/1/9789241598019_eng.pdf,>. ISBN 978-92-4-159801-9.
- ↑ SOMMER, A. Vitamin A deficiency and its consequences [online] . 1. edition. Geneva : WHO, 1995. 69 pp. Available from <http://whqlibdoc.who.int/cgi-bin/repository.pl?url=/publications/1995/92415447783_eng.pdf>. ISBN ISBN 92 4 154478 3.
- ↑ }}