Viral meningitis
From WikiLectures
Viral meningitis is the most common viral infection of the CNS along with inflammation of the soft envelope of the brain (leptomeningitis). Aseptic meningitis includes, in addition to viral meningitis, other forms of meningitis where culture does not reveal the causative agent. The incidence of viral meningitis is difficult to monitor, but it is reported to affect about 1 in 3000 patients with viremia .[1]
Etiology[edit | edit source]
The most common causative agents are
- enteroviruses - currently more than 85% of cases),
- mumps virus,
- HSV 2,
- EBV,
- rarely lymphocytic choriomeningitis, AIDS.
Pathogenesis[edit | edit source]
The viral pathogen can enter the CNS in 2 ways: hematogenously (most common) and neurogenically (typical of herpesviruses)[1];
- In the spring period, young patients are affected by mumps virus; parotitis can be complicated by meningitis, there is also a possibility of residual hearing loss;
- mononucleosis is caused by EBV, affects adolescents, may be complicated by serous meningitis, monocytosis in the blood count, increased fatigue lasting several months!;
- enteroviral infections (caused by ECHO viruses) occur seasonally in adolescents in the summer and autumn, spread by the fecal-oral route, mainly affect the children under one year of age, more common in lower social groups;
- Coxsackie viruses cause C-viruses with severe muscle pain;
- HSV 2 is responsible for 5% of viral meningitis, ¼ of these patients have primary genital infection;
- lymphocytic choriomeningitis is spread by airborne transmission from rodent feces;
- HIV infection is thought of in high-risk groups; HIV antibodies appear 1-3 months after the onset of illness.
Clinical signs[edit | edit source]
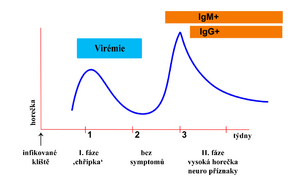
- 1) Prodromal phase (flu) - fever, muscle and throat pain, diarrhoea, exanthema, fatigue and malaise; lasts 3-7 days
- Latency phase - 2-5 days with virtually no difficulties
- 2) Neuroinfection phase - photophobia, headache, nausea to vomiting, dizziness, meningeal symptoms, somnolence;
- recovery usually within 2 weeks;
- some cases may proceed asymptomatically or only through the first phase.
Pathological-anatomical pattern[edit | edit source]
- Inflammation causes edema, engorgement of the meninges and their infiltration by lymphocytes;
- it also affects the surface of the brain (spinal cord).
Differential diagnosis[edit | edit source]
- Subacute onset distinguishes a group of clinically severe meningitis;
- Tuberculous and mycotic meningitis, leptospirosis, sarcoidosis, meningocarcinomatosis, partially treated bacterial meningitis;
- the mild, easy course and spontaneous recovery of acute meningitis differs from the severe course and prognosis of these subacute and chronic meningitis.
Auxiliary examinations[edit | edit source]
- CSF from Lumbar puncture fluid: proteinocytological association, predominance of lymphocytes over monocytes, mild proteinorachia;
- Virus culture from: CSF (early collection), nasal swab, throat swab, stool;
- rise in serological titres in the acute phase of the virus compared to convalescence;
- sedimentation usually normal, leukocytosis at most mild;
- the course of the disease mild;
- virus identification fails in about 20-40%.[2]
Treatment[edit | edit source]
- Symptomatic and supportive with rest and vitamin supplementation;
- acyclovir i.v. - when HSV type 1 or 2 is detected;
- prognosis is always good (self-limiting disease with complete recovery in 7-10 days).
References[edit | edit source]
Related articles[edit | edit source]
- Meningitis
- Serous meningitis and meningoencephalitis
- Herpetic meningoencephalitis
- Suppurative meningitis
- Haemophilic meningitis
- Tuberculous meningitis
- Infectious diseases of the brain
- Neuroinfections, CNS/PGS inflammation
- Encephalitis
Used literature[edit | edit source]
- BENEŠ, Jiří. Infekční lékařství. 1. edition. Praha : Galén, c2009. ISBN 978-80-7262-644-1.