Urine examination
Urine is an easily available biological fluid, the analysis of which provides valuable information about the state of the organism and its metabolism. Urine examination is one of the basic clinical and biochemical procedures that significantly contribute to the diagnosis, monitoring of the disease and treatment results. Urine analysis uses a range of methods, from the simplest color and clotting tube reactions to sophisticated and automated methods such as flow cytometry or immunochemical analysis. Thanks to diagnostic strips, basic examinations can be performed not only in the laboratory, but directly in surgeries or at the patient's bedside.
Urine collection
An important prerequisite for valid urine analysis results is the correct procedure for its collection and collection.
First morning urine
The first morning urine is best for most urine tests. It is recommended that urine collection be preceded by a supine position of at least eight hours. Morning urine is more concentrated and acidic. It is especially suitable for chemical examination of urine. Urine collected later is already affected by fluid intake, food and exercise.
Urine is usually obtained by spontaneous micturition . The actual urine collection is performed after thorough washing and drying of the external urethral orifice. Urine in a clean, dry, closable container that contains no detergent or disinfectant residues that distort the results of the chemical analysis. The middle urine flow is intended for examination. The first stream is always contaminated with cells and bacteria from around the outer urethra. Therefore, the patient urinates the first portion of urine into the toilet and captures the second stream of urine in the collection container, in which the analysis is performed.
In certain situations, urine is collected by suprapubic puncture or by bladder catheterization.
In women, we avoid examinations in the period just before menstruation until the end of menstruation. Stabilizing additives are not required for most qualitative and semi-quantitative chemical analyzes of urine by test strips. If it is not possible to perform the examination within 2 hours after collection, it is advisable to store the urine in a refrigerator or preserve it.
Second morning urine
The sample is soaked 2-4 hours after the first urination. Its composition is already affected by food and fluid intake and exercise. The second morning urine is recommended mainly for quantitative determinations related to the concentration of creatinine in the urine.
Random urine sample
A random urine sample is a label for fresh urine collection without knowledge of collection time and volume, and details of patient preparation are not usually known. It is possible for acute conditions. Urine analysis can be fraught with a number of errors.
Urine collection
For quantitative analyzes and to determine the clearance of different analytes, urine should be collected at intervals. Short-term urine collection lasts 1-3 hours, long-term 12-24 hours. Urine is sometimes collected overnight (for 8 hours), eg to determine albuminuria. The accuracy of the collection is very important for the test results. The accuracy of urine collection can be roughly checked by determining the concentration of creatinine in the urine.
Urine is collected in well-cleaned containers stored in a cool, dark place, or with the addition of a preservative.
Collection can be started at any time during the day by emptying the bladder and recording the time. However, for a 24-hour collection, the best time in the morning is between 6 and 7 o'clock. At the beginning of the urine collection, the patient must urinate; this portion is not yet collected. From that moment on, all the urine is collected. The patient should be instructed to urinate in the collection container before going on the stool. Urine collection is completed in exactly 24 hours by urinating the entire contents of the bladder into a collection container.
Urine volume is measured at the end of the urine collection, the urine is mixed thoroughly, and at least 5 ml of an average sample is usually delivered to the laboratory with the exact time of the start and end of the collection (to the nearest minute) and the exact volume of urine collected.
Physical urine examination
__ Physical examination consists of assessing the color of urine, its odor , foam and turbidity . An important part of the physical examination is the determination of pH , density and osmolality . For the purpose of functional examinations, it is necessary to measure the volume of urine for a precisely defined period of time.
Volume
Daily urine volume is significantly affected by fluid and dietary intake. Volumes less than 400 ml / 24 hours and greater than 2500 ml / 24 hours are considered pathological.
Oliguria and anuria
Oliguria is indicated for urine volume <400 ml / 24 hours and anuria for urine volume <100 ml / 24 hours.
Oliguria and anuria are the basic symptoms of kidney failure. The cause may be dehydration from insufficient fluid intake or increased fluid loss (diarrhea, sweating). Decreased urine volume may be due to primary damage to the renal parenchyma or due to fluid retention (edema, effusions in body cavities).
Oliguria and anuria can also be caused by mechanical obstruction in the urinary tract (prostatic hypertrophy, wedged stone, tumors in the small pelvis). If the obstruction is located below the bladder, we speak of urinary retention .
Polyuria
By polyuria we mean an increase in daily diuresis above 2500 ml.
There are two types of polyurethane states:
- Polyuria caused by so-called water diuresis .
- Water diuresis is due to a reduction in tubular water resorption in the distal part of the nephron. Tubular resorption and excretion of osmotically active substances is within normal limits. Urine osmolality is lower than serum osmolality. It is always less than 250 mmol / kg H 2 O. Water diuresis is encountered physiologically when a larger volume of water is ingested or, for example, when there is insufficient secretion of antidiuretin (diabetes insipidus).
- Polyuria caused by so-called osmotic diuresis .
- It is caused either by increased filtration of osmotically active substances due to their increased osmotic concentration in the ECT (eg hyperglycemia) or by their reduced tubular resorption. Unabsorbed osmotically active substances "bind" water to each other and the result is a reduction in their tubular resorption. Urine osmolality is higher than 250 mmol / kg H 2 O. Osmotic diuresis is characteristic, for example, of diabetes mellitus or polyuric phase of kidney failure or is result of diuretics.
Color
Fresh urine is amber in color, which is attributed to some bilirubinoids, especially urobilin . The intensity of the coloration depends on the concentration and amount of urine, which is determined by fluid intake and extrarenal output. The first morning urine, which is more concentrated, tends to be darker. Some pathological conditions or ingestion of certain exogenous substances may cause discoloration (eg beetroot, rhubarb). Selected characteristic changes in urine color are listed in the table:
| Color | Causing substance | Occurrence |
|---|---|---|
| yellow to colorless |
| |
| Brown | bilirubin |
|
| green-brown | biliverdin - is formed from bilirubin by oxidation in air |
|
| yellow-orange | carotenoids , riboflavin |
|
| pink to fleshy red ( without haze ) | hemoglobin
myoglobin porfyriny beetroot |
|
| pink to fleshy red with haze | blood in the urine - hematuria
(microscopic hematuria, which can only be detected by chemical or microscopic examination, does not affect the color of the urine) |
|
| Dark brown
(standing in the air deepens the color to black) |
melanin
homogentisic acid |
|
| Light red | urates |
|
Odor
We judge it in fresh urine, because by standing in the light, some parts of the urine decompose and the odor changes. The characteristic odor is caused by some of the diseases listed in the table:
| The nature of the smell | Cause | Occurrence |
|---|---|---|
| Ammonia | the presence of urease-producing bacteria that catalyze the decomposition of urea to ammonia and carbon dioxide |
|
| Acetone (overripe apples) | urinary acetone excretion in ketoacidosis |
|
| Maple syrup or maggi spice | branched chain carboxylic oxoacids (especially 2-oxoisocaproic acid , 2-oxoisovaleric acid ) |
|
| hydrogen sulfide to putrefactive | bacterial breakdown of proteins releases H 2 S from sulfur-containing amino acids |
|
| Mouse | phenylacetate |
|
Foam
Normal urine foams little, the foam is white and quickly disappears. The more abundant, colorless, more persistent foam occurs in proteinuria. In the presence of bilirubin , the urine foam turns yellow to yellow-brown.
Turbidity
Fresh urine is usually clear. Turbidity, which occurs after prolonged standing, causes epithelium and has no pathological significance. Turbidity in fresh urine can be caused by the presence of bacteria, leukocytes, lipids, phosphates, carbonates, uric acid, leucine, tyrosine a oxalates. It can be distinguished chemically or microscopically.
Density
Also specific weight in the literature .
Relative density (also relative specific gravity ) is given by the mass concentration of all solutes excreted in the urine. In contrast to osmolality in addition to the number of dissolved particles, it also depends on their molecular weight. High molecular weight substances affect density to a greater extent than electrolytes. In the case of more pronounced glucosuria or proteinuria, the relative specific gravity increases. A protein concentration of 10 g / l increases the relative specific gravity of urine by 0.003 and a glucose concentration of 10 g / l by 0.004. The relative specific gravity of urine depends significantly on temperature.
By relative urine density we mean the ratio of urine density to water density. The density of water is practically equal to 1 kg / l, so the difference between the density of water (in kg / l) and the relative density of urine is negligible. The density in the SI system is kg · m -3 . The density of the sample relative to the density of water is a relative quantity and is therefore given by a dimensionless number.
Determination of urine density
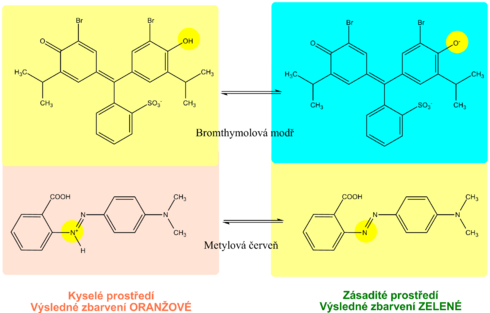
Urine density is estimated indirectly from cation concentrations using diagnostic strips. The indicator zone of the strip contains a suitable polyelectrolyte as an ion exchanger and the acid-base indicator bromothymol blue. The principle of diagnostic strips is based on the exchange of cations from urine, especially Na + , K + , NH 4 + , for H + polyelectrolyte ions in the indication zone. The released H + acidifies the weakly buffered acid-base indicator, which is in alkaline form. Acidification is accompanied by a change in the color of bromothymol blue. The disadvantage is that the examination with diagnostic strips does not take into account non-electrolyte substances such as glucose , proteins, urea ,creatinine and some others.
Under physiological conditions, urine density ranges from 1,015 to 1,025. Extreme values of 1,003-1,040 can be reached in the dilution and concentration experiment .
As a rule, the larger the volume of urine, the lower its density (diluted urine) and, conversely, the smaller the volume of urine (concentrated urine), the higher. Conditions in which osmotic diuresis deviates from this rule : for example, in diabetes mellitus , the volume of urine is larger with a higher specific weight.
Density determination allows an approximate estimation of renal concentration. Values above 1,020 and higher are indicative of good renal function and the ability of the kidneys to excrete excess solutes. Highly concentrated urine indicates a significant reduction in circulating plasma volume.
When the kidneys are unable to concentrate urine, low-concentrated urine of low specific gravity is excreted; we are talking about hypostenuria . The patient excretes the same amount of solids with higher water consumption. Extremely diluted urine may be a symptom of impaired renal concentration, such as diabetes insipidus , or due to the side effects of some medications. The combination of hypostenuria with polyuria indicates damage to the renal tubular system.
Isostenuria is a serious symptom of kidney damage . The kidneys lose the ability to concentrate (and dilute) urine and excrete urine with the same density as the glomerular filtrate. The relative density of urine remains consistently low, at about 1,010. The current finding of isostenuria with oliguria is an indicator of severe renal insufficiency.
Dehydration , proteinuria or glycosuria contribute to the increase in relative density - hyperstenuria .
| Designation | Relative density | Causes |
|---|---|---|
| Eustenuria | 1,020-1,040 | |
| Hyperstenurie | > 1,040 |
|
| Hypostenurie | <1,020 |
|
| isosthenuria | 1,010 th most common |
|
Osmolality
Urine osmolality depends on the amount of osmotically active particles excreted in the urine, regardless of their weight, size or electric charge. Osmolality is expressed in mmol/kg. It is only approximately dependent on urine density. Its measurement is more accurate compared to density, has a greater informative value and is preferred.
If we compare the two quantities, the osmolality reflects the total mass concentration of all solutes, while the density reflects their total mass concentration. Therefore, we can simply say that osmolality will be more affected by changes in the concentration of low molecular weight substances (in practice, especially sodium, glucose and urea), while density will be more significantly affected by the presence of protein in the urine.
Normal osmolality values at normal fluid intake are 300-900 mmol / kg. Urine osmolality depends on the dilution and concentration of the kidneys. The extreme values of osmolality at maximum dilution or maximum concentration are in the range of 50-1200 mmol / kg. If the osmolality of the urine is approximately the same as the osmolality of the blood, it is isoosmolar urine. Hypoosmolar urine has a lower osmolality than blood, i.e. less than about 290 mmol/kg. Hyperosmolar urine is urine with a higher osmolality than blood.
Theoretically, we can imagine that definitive urine arises from isoosmolar glomerular filtrate, to which pure, so-called solvent-free water is added or resorbed in the renal tubules.
The transport of solute-free water expresses its clearance. We will explain what this quantity means using the following considerations: First, let us define the clearance of osmotically active substances. It is a quantity analogous to the commonly used clearance of endogenous creatinine: the clearance of osmotically active substances represents the theoretical volume of blood plasma, which is completely deprived of all osmotically active particles in the kidneys per unit time. The following will apply (derivation is similar to endogenous creatinine clearance):
- ,
| where | Closm | is the osmolar clearence in ml/s, |
| V | is diuresis in ml/s | |
| Uosm | is the osmolar urine concentration in mmol/kg of water, | |
| Posm | is the osmolar plasma concentration v mmol/kg of water. |
If the primitive urine has the same osmolality as the plasma and we neglect the contribution of proteins to the total osmolality of the plasma, the volume of filtered primitive urine must be the same as the clearance of the osmotically active Cl particles .
Solvent-free water clearance is the difference between the actual volume of definitive urine excreted per unit time and osmolar clearance:
| where | ClH2O | is the clearence of solute-free water in ml/s, |
| Closm | is the osmolar clearence in ml/s, | |
| V | is diuresis in ml/s. |
If the clearance of solute-free water is negative, it means that part of the solute-free water has been resorbed from the primitive urine, so that the definitive urine is more osmotically concentrated. Conversely, if the clearance of solute-free water were positive, hypoosmolar urine would form, against blood plasma diluted with solute-free water. Physiological values range between ,00.027 and ,000.007 ml / s.
The kidneys are able to excrete large amounts of solute-free water to prevent hyponatremia. Conversely, in the absence of water, its excretion is limited and particles are excreted in a smaller volume of water.
Determination of the urine osmolality
With osmometer
Osmometers are used to accurately determine osmolality. They take advantage of the fact that dissolved particles affect some properties of the solution:
- they reduce the freezing point of the solution (cryoscopic principle);
- they increase the boiling point of the solution (ebulioscopic principle);
- they reduce the solvent vapor pressure above the solution.
The magnitude of the change in the above quantities depends on the concentration of osmotically active substances in the measured solution, and osmometers record these changes with great accuracy. A lowering of the freezing point is usually detected. It is true that 1 mol of particles of a substance dissolved in 1 kg of water lowers its freezing point by 1.86 °C.
Roughly by calculation based on the substance concentration values of Na+, K+, NH4+ and urea in urine
- Urine osmolality = 2([Na+] + [K+] + [NH4+]) + [urea]
This calculation fails if the urine contains a high concentration of other substances, which are physiologically present in orders of magnitude lower amounts - for example, with significant glycosuria or ketonuria.
Roughly calculated from the relative density value
- If the urine does not contain protein or sugar
- we multiply the last two digits of the relative density value by a factor of 33.
- If the urine contains protein or sugar
- we must first correct the relative density value
- in the presence of protein, we subtract 0.003 from the relative density value for every 10 g/l;
- in the presence of glucose, we subtract 0.004 from the relative density value for every 10 g/l.
Examination of kidne concenration
Impaired renal impairment is one of the first signs of renal disease. We proceed with its investigation as follows:
- We first examine the osmolality in the morning urine sample . A healthy person should produce urine with an osmolality of about 600 mmol / kg after taking fluids at night . This value indicates good renal concentration and, if achieved, we do not proceed with further investigation.
- The adiuretin test reflects the ability of the distal tubule and collecting duct to respond to adiuretin (vasopressin) by producing concentrated urine. The patient is administered 10 μg (2 drops) of 1-deamino-8-D-arginine vasopressin ( DDAV ), a synthetic analogue of adiuretin, to each nostril after nocturnal withdrawal . It is characterized by an enhanced antidiuretic effect, while other pharmacological effects are suppressed. The patient collects urine at four one-hour intervals and the osmolality of individual urine samples is measured. If it exceeds the value given in the table, this indicates good renal concentration and we will terminate the experiment. At the same time as the urine, blood is collected and the serum osmolality is examined. From the values of osmolality in urine and serum, we calculate the osmotic index (U osm(S eight ), which more accurately reflects the concentration capacity of the kidneys.
Physiological values of urine osmolality and osmotic index after adiuretin administration Věk Ummol/kg H2O Uosm/Sosm 15–20 970 3,34 21–50 940 3,24 51–60 830 2,86 61–70 790 2,72 71–80 780 2,69
Another possibility is to evaluate urine osmolality under conditions of varying lengths of fluid withdrawal, which are currently rarely performed.
The concentration ability of the kidneys is impaired mainly in diseases affecting the renal tubules and interstitium, where the countercurrent concentration gradient is disturbed.
It is also possible to examine the dilution ability of the kidneys after exposure to distilled water. The test reflects the ability to produce urine whose osmolality is significantly lower than the osmolality of the serum.
pH
__
The kidneys are the organ where the acid-base balance is adjusted by eliminating (or retaining) H + . The pH in the glomerular filtrate is the same as in plasma. As it passes through the renal tubular system, urinary acidification occurs.
The concentration of free protons in the urine is negligible compared to other ions; we can therefore say that H + is eliminated by the kidneys in two forms:
- bound to the anions present, eg to phosphates (conversion of hydrogen phosphate to dihydrogen phosphate)
- H+ + HPO42- → H2PO4-
- or to the anions of certain organic acids. This proportion is called the so-called titratable acidity, which under normal conditions is 10-30 mmol / 24 hours. It can be determined by titration with sodium hydroxide.
- as the ammonium cation, which is the most important system.
- H + + NH 3 → NH 4 +
- The amount of NH 4 + excreted in the urine is between 30-50 mmol / 24 hours.
Urine pH depends on:
- on the composition of the diet
- In a healthy person, urinary pH is most affected by the composition of the diet. Lactovegetarian diet causes alkalization of urine. In contrast, a diet rich in protein (meat) is accompanied by acidification.
- on the state of acid-base equilibrium
- Under pathological circumstances, urine pH reflects acid-base imbalances. Changes in urine pH are a manifestation of the compensatory and corrective activity of the kidneys. Aciduria is the result of correction of metabolic and correction of respiratory acidosis, alkaliuria is at the beginning of compensation of respiratory and correction of metabolic alkalosis. However, the excretion of acidic urine in acidosis and alkaline urination in alkalosis only applies to mild disorders and well-functioning kidneys. The current finding of aciduria and ketonuria indicates starvation. A combination of aciduria, ketonuria and glycosuria is common in the decompensation of diabetes mellitus.
The most common factors affecting urine pH Acidic pH Alkaline pH protein diet vegetarian food protein diet vegetarian food dehydration renal tubular acidosis diabetická ketoacidóza respiratory and metabolic alkalosis metabolic and respiratory acidosis bacterial urinary tract infections starvation
Permanently alkaline urine pH may indicate:
- Infection of the kidneys or urinary tract with urease-producing bacteria. Enzymatic hydrolysis of urea produces ammonia, which alkalizes the urine. The situation is similar for bacterially contaminated urine, in which the bacteria multiplied during a longer period of storage.
- H 2 N-CO-NH 2 + H 2 O2NH 3 + CO 2
- NH3 + H2O → NH4+ + OH-
- Distal renal tubular acidosis , which is a disorder of the renal tubular cells characterized by the inability of the distal tubule to secrete H + .
The main benefit of urine pH testing is in the diagnosis and treatment of urinary tract infections and urolithiasis . Permanent variations in urine pH may be one of the factors contributing to the formation of urinary stones.
- Calcium oxalate stones are common in acidic urine. At acidic pH, uric acid stones are also easily formed. Alkalization of urine above pH 7.0 can, under favorable circumstances, lead to the slow dissolution of uric acid stones and the prevention of their formation. Cystine also precipitates more easily in acidic urine.
- Phosphates are poorly soluble in alkaline urine and at pH above 7 ammonium magnesium phosphate (struvite - MgNH 4 PO 4 · 6H 2 O) and a mixture of phosphate and calcium carbonate ["carbonate capatite" - Ca 10 (PO 4 CO 3 OH ) 3 (OH) 3 ].
Determination of urinary pH
Urine pH should always be tested in fresh urine. It is usually determined by diagnostic strips . Accurate pH determination can be performed with a pH meter .
The physiological pH of urine is in the range of 5.0–6.5, the extreme values are 4.5–8.0. Extreme values in the acidic or alkaline range suggest that urine collection instructions are not followed.
Examination of renal acidification
The basic examination to assess the acidifying activity of the kidneys is to examine the pH of a morning urine sample . The pH determination must be performed immediately and the use of a pH meter is recommended . In a healthy adult, the pH of the morning sample is less than 6.0. At higher values, there is a suspicion of impaired acidification, and if there are no contraindications (eg significant reduction in renal function), it is possible to perform an acidification test after NH 4 Cl or CaCl 2(in patients with hepatic impairment). The patient is given ammonium chloride (2 mmol per kg body weight). 3 hours after ingestion of the test substance, urine is collected at 3-hour intervals and immediately after collection, the acidity of the urine samples is measured with a pH meter. With intact renal acidification, urine pH should fall below 5.5.
Acidifying ability is impaired in patients with renal tubular acidosis of the distal type.
In the case of an ambiguous result of the acidification test, the alkalizing ability of the kidneys after oral or intravenous exposure to sodium bicarbonate is examined.
Chemical examination of urine
__Protein , glucose , hemoglobin , ketone bodies and bile pigments are routinely detected in urine . These components are usually found in the urine of healthy people, but in such small amounts that we do not prove them by routine tests. In various pathological conditions, their concentration in urine increases.
Tube reactions
__ Chemické vyšetření moči mokrou cestou
Test (diagnostic) strips
Detection of pathological components of urine directly at the patient's bedside or in the line of first contact with the patient enables examination using test strips.
The test strips consist of a plastic carrier on which one or more indication zones are mounted. These are manufactured in such a way that a liquid analytical reagent is sucked into a suitable material (eg special filter paper) and gently dried.
Diagnostic strips are available as monofunctional , multifunctional or special examination strips .
Monofunctional strips contain basic indication zones for semi-quantitative determination of a substance in urine. Polyfunctional strips are formed by several indication zones, enabling examination of several biochemical parameters at once. They are intended for cases where it is necessary to obtain as much information as possible about the patient's health condition, eg at various screening events. In addition to monofunctional and polyfunctional strips, there are special test strips that include combinations of two or more indication zones that are selected for a particular disease, e.g., diabetes mellitus screening strips contain a zone for glucose, ketone bodies, protein, and pH.
The following urine parameters can be determined using test strips:
Principles of determining individual parameters
Protein
__
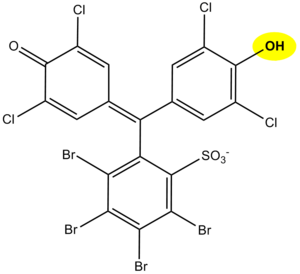
The principle of determination of proteins in urine using diagnostic strips is based on the so-called protein error of an acid-base indicator , eg tetrabromophenol blue , tetrabromophenolphthalein ethyl ester or 3´, 3´´, 5´, 5´´-tetrachlorophenol-3,4,5,6- tetrabromosulfophthalein. Like any acid-base indicator, these substances change color at a certain pH (they behave like weak acids, while the protonated form has a different color than the dissociated form): at pH below 3.5 they are yellow, at higher pH they are green to blue. In addition to the indicator, there is a buffer in the reaction zone of the test strip, which maintains the pH in the range of 3.0 to 3.5, so the indicator is yellow. If there are proteins in the sample, they bind to the indicator with their amino groups. However, this changes its properties - the transition area shifts towards a more acidic pH. This means that at the stated constant pH between 3.0 and 3.5, the protein-bound indicator will be green, as if it were in a more alkaline environment (hence the protein error of the indicator ).). The color intensity depends on the protein concentration, varies from green to blue and is evaluated visually or instrumentally.
In highly alkaline urine (pH above 8) or if the urine is very concentrated, the test may give false positive results (buffer will be depleted in the reaction zone). In these cases, acidify the urine with a few drops of dilute acetic acid to pH 5-6 and repeat the test. False positives can also be caused by high concentrations of some substances with amino groups (contamination of the sampling vessel with some disinfectants), which bind to the indicators similarly to proteins.
The disadvantage of the test strips is their different sensitivity to individual proteins. The strips react very well with albumin and indicate its presence in urine from 0.1 to 0.5 g / l. They are significantly less sensitive to globulins, glycoproteins and Bence-Jones protein . These diagnostic strips do not show an increase in albuminuria to values up to about 200 mg / l, resp. daily albumin losses in the range of 30 to 300 mg / 24 hours, which accompanies especially the earlier phases of some nephropathy. Immunochemical methods can be used to screen for increased albuminuria, such as special diagnostic strips based on immunochromatographic principles or immunoturbidimetry.
Hemoglobin
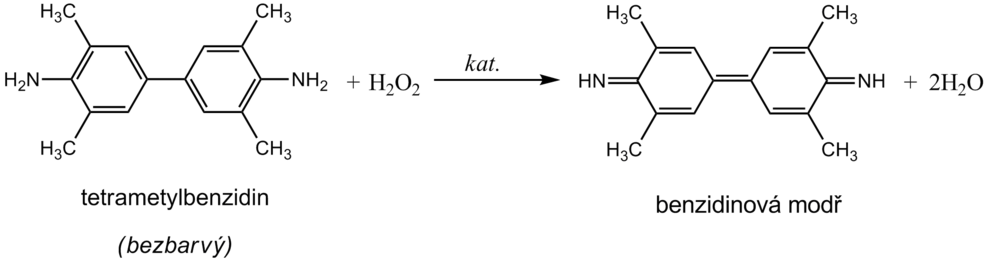
__ Hemoglobin catalyzes, like peroxidase , the oxidation (dehydrogenation) of some substrates (eg benzidine derivatives ) by hydrogen peroxide:
However, it is not an enzyme activity (catalysis is conditioned by heme iron) and therefore it is not lost even after heat denaturation. We are talking about pseudoperoxidase activity , which is used for sensitive but non-specific evidence of hemoglobin or trace amounts of blood. It is preferable to use a chromogenic substrate to monitor the reaction, i.e., a substance that provides a markedly colored product by dehydrogenation (often benzidine or its non-carcinogenic derivatives, aminophenazone, etc.).
The reagent zone of the diagnostic strips contains a chromogen (eg tetramethylbenzidine ) with stabilized hydrogen peroxide (eg cumene hydroperoxide ). In the presence of free hemoglobin ( hemoglobinuria ), the indication zone turns uniformly blue. If erythrocytes ( erythrocyturia ) are present in the urine , intensely green-blue dots to spots form.
Hemoglobinuria can be encountered in intravascular hemolysis . Damage to the glomerular membrane ( glomerular hematuria ) and bleeding from any part of the urinary tract lead to more frequent erythrocyturia . It is often found in urinary tract infections , urolithiasis and urogenital tract tumors .
In addition to hemoglobin , myoglobin also provides a pseudoperoxidase response , which can be excreted in the urine during skeletal muscle breakdown ( rhabdomyolysis , crush syndrome ). The positivity of the test may also be due to peroxidases of leukocytes or certain bacteria, yeasts or fungi, which may occur in the urine, especially in urinary tract infections . To rule out the possibility of a false positive reaction due to cellular peroxidases, the reaction must be performed with boiled urine.
Contamination of the sampling vessel with strong oxidizing agents also causes a false positive reaction. On the other hand, the presence of strong reducing substances (eg ascorbic acid ) can slow down or even stop the pseudoperoxidase reaction and thus cause false negative results.
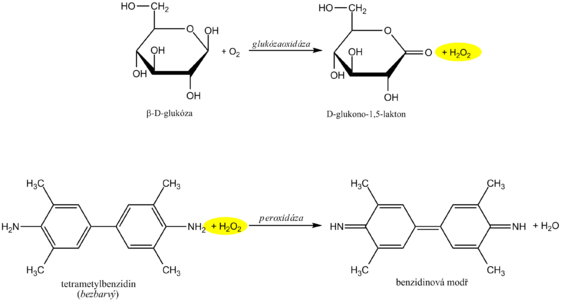
Glucose
__
Diagnostic strips for the detection of glucose in urine are based on the principle of enzymatic reactions with glucose oxidase and peroxidase (same principle as the determination of glycemia ). D -glucose is oxidized by oxygen using glucose oxidase to form D -glucono-1,5-lactone and hydrogen peroxide. In a subsequent peroxidase reaction, hydrogen peroxide oxidizes tetramethylbenzidine or another chromogen to a colored product. The light yellow color of the reaction surface changes to blue-green when positive. The test is specific for D -glucose, other sugars do not give a positive reaction.
High concentrations of reducing agents such as ascorbic acid slow down the development of color and can lead to falsely lower results. In these cases, it is recommended to repeat the analysis at least 10 hours after vitamin C withdrawal. Conversely, false positive results may be due to the presence of peroxidase substrates or oxidizing agents in the sampling vessel (eg H 2 O 2 , Persteril ®, chloramine B ). Urine glucose determination should be performed rapidly to avoid bacterial contamination or urine should be stored at 4 ° C.
Interference with ascorbic acid is a common source of false negatives. Urine test strips from some manufacturers are therefore modified so that the reaction zone is at least somewhat resistant to ascorbic acid. Some diagnostic strips also have an ascorbate detection zone to alert you to false negatives.
Glucosuria is most often accompanied by an increase in glycaemia above the so-called renal glucose threshold (around 10 mmol / l). Glucose, which normally filters through the glomerular membrane, is in such a high concentration in primitive urine that it is not enough to be resorbed in the tubules and reaches the final urine. Glucosuria with normal glycemia indicates a disorder of tubular transport mechanisms - we are talking about renal glucosuria .
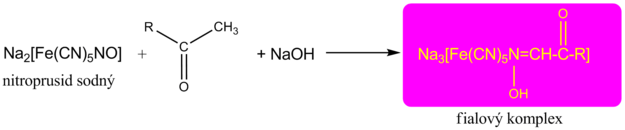
Ketons
__ The detection of ketone bodies is based on the reactions of acetoacetic acid and acetone with sodium nitroprusside in an alkaline medium, which forms a red-violet-colored complex . This principle is used by Legal's and Lestradet's exams , as well as diagnostic strips. Β-hydroxybutyric acid (ie the most abundant ketone substance) does not provide a reaction and therefore a negative result does not completely rule out ketoacidosis.
Compounds with free sulfhydryl groups (eg the antihypertensive captopril or uroprotectant used in some mesna chemotherapeutic regimens ) provide false positivity for urinary ketone bodies . Quite often, bacterial products in urinary tract infections also provide a similar response.
False negatives , apart from the already mentioned insensitivity of the β-hydroxybutyric acid tests, are not significant.
Bilirubin
__ Detection of bilirubin in urine by diagnostic strips is based on the azocoupling reaction provided by conjugated bilirubin with a stable diazonium salt (eg 2,6-dichlorobenzenediazonium tetrafluoroborate ). A pink to pinkish-red dye is formed. When high concentrations of urobilinogen occur, the color changes to orange. In this case, it is recommended to evaluate the coloration up to 2 minutes after the indication zone has wetted. Lower to false negative results may be due to high concentrations of ascorbic acid . Urine specimens should be protected from direct sunlight, which causes oxidation of bilirubin, followed by a falsely inferior to negative finding.
Only conjugated bilirubin is examined in the urine , as unconjugated bilirubin cannot be excreted in it.
Urobilinogen
__ As with bilirubin, the principle of azocoupling reaction with a stable diazonium salt (eg 4-methoxybenzenediazonium tetrafluoroborate) is used to determine urobilinogen in urine . The indication zone turns pink to red in the presence of urobilinogen. The faint pink color still corresponds to the physiological excretion of urobilinogen. In the presence of bilirubin , the color is yellow, which turns green to blue after 1 minute.
Some heterocyclic nitrogenous substances produced by bacteria in urinary tract infections can cause false positives . High concentrations of ascorbate can cause false negatives .
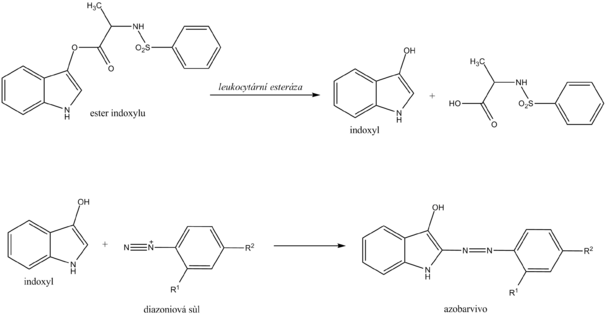
Leukocytes
__ Chemical determination of leukocytes with a diagnostic strip is based on the detection of esterases that are abundant in granulocytes . Granulocyte esterases catalyze the hydrolysis of indoxyl ester to free indoxyl. The indoxyl then reacts with the stable diazonium salt to form the appropriate azo dye. In the case of a negative reaction, the zone turns cream yellow; in the case of a positive reaction, it changes to a pink to purple hue.
Chemical examination of leukocytes does not replace microscopic examination . On the other hand, it is possible to detect lysed leukocytes (eg in hypotonic urine ) in this way, which is not possible with microscopic examination.
Leukocyturia is a symptom of inflammation of the kidneys or urinary tract. The cause of most positive findings is a bacterial infection of the urinary tract . In case of a positive leukocyte finding, it is recommended to supplement the examination of proteinuria , hematuria , nitrituria , examination of urinary sediment and further microbiological examination .
Dusitans
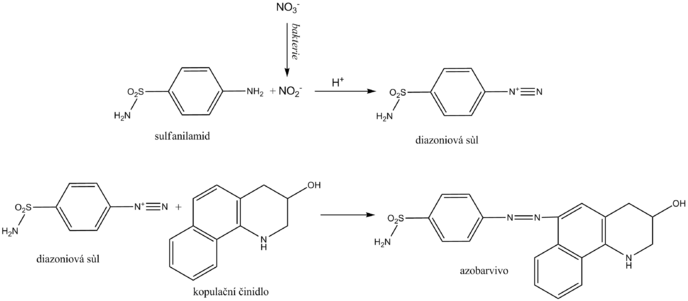
__ Nitrite is determined in the urine as an indirect sign of bacteriuria . Normal urine does not contain them in measurable concentrations. Some primarily gram -negative bacteria , such as Escherichia coli , Proteus , Klebsiella , staphylococci and others, have the ability to reduce the nitrates present in the urine to nitrite. Diagnostic strips for indirect detection of bacteriuria use nitrite in the so-called Griess reaction . Its essence is the diazotization of sulfanilamide with nitrite in the sample to form the diazonium salt. This is followed by azocoupling of the resulting salt with a coupling agent, developing a pink to purple color.
The nitrite urine test should be performed in the first morning urine, as in this case a sufficiently long time is guaranteed for the bacterial reduction of nitrates to nitrite in the bladder. Another recommendation is to consume enough vegetables (contains nitrates) the day before the examination. A positive urinary nitrite test confirms bacteriuria, while a negative one does not excrete it.
Indirect evidence of bacteriuria is indicative and does not replace microbiological examination.
Ascorbic acid
__ Ascorbic acid appears in the urine with high food intake. As a strong reducing agent, it can affect the determination of some analytes in urine, especially those that use hydrogen peroxide in the reactions. It is directly reduced with ascorbic acid. It also rapidly degrades diazonium salts used for azocoupling reactions.
The principle of ascorbic acid detection uses phosphomolybdic acid, which is reduced to molybdic blue by ascorbic acid. The reaction is not only specific for ascorbic acid, other substances with strong reducing effects react similarly.
pH
__
The pH indication zone contains a mixture of selected acid-base indicators. Most use two acid-base indicators - methyl red and bromothymol blue, or phenolphthalein . This ensures that the pH is read in the range 5-9 by changing the color from orange (acidic pH) to green to blue (alkaline pH). The reading is possible with an accuracy of 0.5.
Density
__ By relative urine density we mean the ratio of urine density to water density. The density of water is practically equal to 1 kg / l, so the difference between the density of water (in kg / l) and the relative density of urine is negligible. The density in the SI system is kg · m -3 . The density of the sample relative to the density of water is a relative quantity and is therefore given by a dimensionless number.
Determination of urine density
Urine density is estimated indirectly from cation concentrations using diagnostic strips. The indicator zone of the strip contains a suitable polyelectrolyte as an ion exchanger and the acid-base indicator bromothymol blue. The principle of diagnostic strips is based on the exchange of cations from urine, especially Na + , K + , NH 4 + , for H + polyelectrolyte ions in the indication zone. The released H + acidifies the weakly buffered acid-base indicator, which is in alkaline form. Acidification is accompanied by a change in the color of bromothymol blue. The disadvantage is that the examination with diagnostic strips does not take into account non-electrolyte substances such as glucose , proteins, urea ,creatinine and some others.
Procedure for examination with diagnostic strips
We will only remove as many strips from the tube as we need immediately. Close the tube with the remaining strips immediately to protect the unused strips from moisture. We do not touch the strip zone with your hands. We store the strips only in the original packaging and well closed with a bag of desiccant, in the dark, in a dry place at a temperature of +2 to +30 ° C.
We immerse the strip briefly for 1-2 s in the examined urine so that all zones are wetted. Then remove the strip and remove excess urine by wiping the edge of the strip against the edge of the container. We then place it in a horizontal position to prevent mixing of reagents from the individual reagent pads. After the prescribed reaction time, usually 60 s, the leukocytes are evaluated for 120 s.
Evaluation of the color of the reaction zones of the diagnostic strips is performed:
- subjectively comparing the resulting coloration to the color scale on the tube label in which the strips are stored;
- objectively using reflectance photometers that measure the intensity of light of the appropriate wavelength reflected from the reaction field.
Overview of urine tests using diagnostic strips
| Analyt | Princip | Falešně pozitivní výsledky | Falešně negativní výsledky |
|---|---|---|---|
| Protein | Protein error of acid-base indicator | Alkaline pH, contamination of the sampling vessel with disinfectants based on quaternary ammonium salts, menstruation (not examined 3 days before and after), hemoglobinuria, myoglobinuria | Globulins and immunoglobulin light chains are difficult to detect |
| Hemoglobin | Oxidation of chromogen by hydrogen peroxide due to pseudoperoxidase activity of hemoglobin | Microbial peroxidases, contamination of containers with oxidative cleaning agents | High nitrite concentration, vitamin C |
| Glucose | Glucose oxidase reaction coupled with peroxidase reaction | Contamination of containers with oxidative cleaning agents | Vitamin C, other reducing agents (gentisic acid, DOPA), urinary tract infection |
| Ketons | Reaction of acetoacetic acid and acetone with nitroprusside in an alkaline medium | Substances with free sulphhydryl groups (eg captopril ). Some phenolphthalein and sulfophthalein-based substances (laxatives and diagnostics) provide similar coloration in alkaline environments. Phenylpyruvic acid | β-hydroxybutyrate does not react |
| Bilirubin | Azocoupling reactions | Substances that have a similar color in an acidic environment, nitrogenous metabolites of bacteria in some urinary tract infections | High nitrite content, light exposure, ascorbic acid |
| Urobilinogen | Azocoupling reactions | Substances that have a similar color in an acidic environment, nitrogenous metabolites of bacteria in some urinary tract infections | Formaldehyde, light exposure, old urine, ascorbic acid |
| Dusitans | Griess reaction - diazotization of sulfanilamide with nitrite and subsequent azocoupling | Bacterial contamination | Dietary nitrate deficiency, Gram-positive bacteria, major diuresis, vitamin C |
| Leukocytes | Esterase activity of granulocytes and macrophages | Formaldehyde, alkaline pH, high urine density | Vitamin C, some drugs |
| pH | A mixture of acid-base indicators | Formaldehyde (seemingly lower pH), old urine (alkaline pH) | |
| Density | Ion exchange of urine cations for H + , determination of pH by acid-base indicator | Alkaline pH pushes the results to lower values |
Examination of urinary sediment
__
Morphological components of urine can be detected by microscopic examination of the urinary sediment and, more recently, by flow cytometry .
Urine sediment analysis is not a screening procedure. We approach its analysis in the following indications:
- in case of a positive finding of a chemical examination of the urine (positive erythrocytes , protein , nitrites );
- if the leukocyte test is positive with diagnostic strips;
- in clinical suspicion of kidney and urinary tract disease;
- during follow-up examinations of patients with nephrological or urological diseases.
Orientation examination of urinary sediment
As an indication , erythrocytes, leukocytes and bacteriuria can be detected indirectly by the nitrite test (Table 1). If the strips are found to be positive, a more demanding microscopic examination must be performed . However, the use of diagnostic strips will reduce unnecessary microscopic evaluation requirements. The strips are also used when the cell elements break down due to low osmolality or high urine pH , when the sample is standing for a long time or at a higher room temperature. The finding in the urinary sediment is negative, but the presence of disintegrated erythrocytes and / or leukocytes may be indicated by a positive finding when tested with a test strip. Pseudoperoxidase activity of hemoglobinor the activity of leukocyte esterases persists for several hours after release from the cells.
- Tab. 1 Orientation examination of urinary sediment using diagnostic strips
Diagnostic strip (reaction zone) Microscopic equivalent Blood (hemoglobin / erythrocytes) Erythrocytes, erythrocyte cylinders Leukocytes Leukocytes, leukocyte cylinders Protein Hyaline, waxy, granular cylinders Dusitany Bacteria
Microscopic examination of urinary sediment
Microscopic examination procedure
- Urine sample preparation
- A middle stream of the first or second morning urine is taken for microscopic examination of the urine sediment. The second morning urine is recommended because the cell elements in the first morning sample are often damaged or broken. Also, a significant reduction in urine osmolality and alkaline pH reduces the occurrence of formed elements due to their lysis.
- For examination of urinary sediment, it is necessary to process fresh urine within 1 hour after collection. Prolongation of the interval between urine collection and examination of urinary sediment is accompanied by cell breakdown and death.
- Mix the urine sample well and then measure 5 ml or 10 ml of urine into a test tube. Centrifuge at 400 g for 5 minutes, preferably at 4 ° C. Then carefully aspirate 9 parts of supernatant ; that is, the sediment is 10 times concentrated. If we work with a stained preparation (see below), we add the dye in an amount that corresponds to 10% of the total volume.
- Staining procedure
- Dilute 50 μl of the staining solution (alcian blue and pyronin B in a ratio of 1: 1) in 0.5 ml of urine sediment and mix gently.
- After 5 minutes, transfer 13 μl of stained sediment to a slide and cover with an 18 × 18 mm coverslip. A larger volume of stained sample with the appropriate size of coverslip can also be used.
- We first view the sample at a magnification of 100–200 ×, when we can assess the uniform distribution of the elements and notice rare particles such as cylinders and epithelial cells. Then we proceed to the counting of elements at a magnification of 400 × in at least 10 randomly selected fields of view. After conversion to the original urine volume, the results are reported as the average number of particles in 1 μl of urine. Higher accuracy of element counting is achieved by using a chamber ( Bürker or other chamber).
Possibilities of microscopic examination
Transmitted light microscopy and phase contrast techniques are used for microscopic examination of urinary sediment, and in special cases also polarization filter microscopy.
- Transmitting light microscopy
- Allows rough orientation or search for pathological findings. Using light microscopy , unstained specimens may escape hyaline warfare and bacteria during evaluation . Accurate identification of leukocytes, macrophages and renal tubular cells is very difficult in unstained preparations. Supravital staining is recommended for reliable determination of urinary element morphologythat highlights some cellular details. By supravital staining we mean staining a wet unfixed preparation in which some cells still survive. Sternheimer staining using blue and red color contrast with alcian blue and pyronine B is recommended. Due to its strong affinity for mucopolysaccharides, alcian blue stains the surface of cells and elements, pyronin B penetrates inside the cells and stains the cytoplasm in particular.
- Phase contrast microscopy
- It is a suitable method for rapid evaluation of unstained slides. It is used for more detailed assessment of sediment, especially better recognition of leukocytes, cylinders and crystals and differentiation of erythrocytes, including morphological changes of membranes. A better display of details allows you to increase the contrast, which is achieved by shifting the phase of the light wave of part of the rays.
- Polarizing filter microscopy
- It is suitable for better identification of crystals and fat bodies.
Components of urinary sediment and their evaluation
In the urinary sediment, we assess organ components, mainly represented by cells, or cylinders, and non- organs , among which we include crystals. We also notice the presence of microorganisms and various artifacts may occur. The main components of urinary sediment are summarized in Table 2.
- Tab. 2 Overview of the main components of urinary sediment
erytrocyty Cellular elements blood cells erythrocytes leukocytes lymphocytes macrophages epithelium renal tubular cells transitional epithelial cells squamous epithelium tumor cells Rollers cellless hyalinní granular waxy fat cellular erythrocyte leukocytové epithelial bacterial Microorganisms bacteria yeast trichomonády mold Crystals
Cellular elements
Leukocytes
- Polymorphonuclear granulocytes are the most frequently detected . They are round cells (average size 10 μm) with granular cytoplasm. The nucleus is segmented, but is often subject to degenerative changes and in this case is difficult to distinguish from the cytoplasm. Sometimes it stains badly; when stained, it is markedly blue, while the cytoplasm tends to turn red and reddish brown. The appearance of granulocytes is also affected by urine osmolality. They often gather. The finding is characteristic of a urinary tract infection, if erythrocytes are present at the same time, it may affect the glomeruli. Bacteria are also found in about 50% of leukocytes. Eosinophilscan only be demonstrated using special staining. A false positive finding may be due to urinary contamination (vaginal secretion, failure to follow urine collection instructions - first stream).
- The occurrence of lymphocytes in the urine is mostly associated with chronic inflammation of the kidneys , sometimes with viral infections and further with kidney rejection after transplantation . Lymphocytes have a homogeneous nucleus with a thin cytoplasmic margin. The ratio of nucleus to cytoplasm and the smooth structure of the cytoplasm are best distinguished from renal tubular cells.
- Sometimes we can also meet macrophages . Their finding is relatively common in urinary tract infections.
- Reference values
- ≤ 10 leukocytes/μl urine,
- approximately < 5 leukocytes/field of view.
Erythrocytes
- The presence of erythrocytes in the urine is usually a symptom of kidney or urinary tract disease. Erythrocytes are smaller than leukocytes. They appear as non-nuclear discoid bodies with an average size of about 6 μm. In hyperosmolar urine, where erythrocytes easily lose intracellular fluid , their diameter decreases and they become creped to spiny. Conversely, in hypoosmolar urine, fluid enters erythrocytes, enlarges and may disintegrate. With a low hemoglobin content , they are difficult to recognize and appear as so-called shadows.
- From the appearance of red blood cells we can deduce their origin. With significant damage to the glomerular membrane, penetration of not only proteins but also erythrocytes is possible. As the erythrocyte passes through the glomerular membrane, the shape is deformed and the structure changes. Erythrocytes that show deviations from the discoid shape are termed dysmorphic.Sometimes they have the shape of "tires" (so-called ring or annular erythrocytes), other times the membrane of erythrocytes extends into the vesicles, in this case we are talking about acanthocytes. An increased incidence of dysmorphic erythrocytes is typical of renal glomerular involvement. The proportion of dysmorphic erythrocytes in more than 80% indicates glomerular hematuria and we usually find proteinuria at the same time. If isomorphic erythrocytes are present in more than 80%, this is non-glomerular hematuria, where the source of erythrocytes is bleeding from the urinary tract or bleeding from ruptured blood vessels in kidney tumors or urolithiasis. Phase contrast microscopy is required to identify dysmorphic erythrocytes.
- The causes of haematuria must always be clarified, in particular cancer or severe glomerulopathy ( glomerulonephritis ) must be ruled out.
- The cause of the increased number of erythrocytes in the urinary sediment can also be extreme physical exertion, the use of anticoangulants or the admixture of menstrual blood .
- Reference values
- < 5 erytrocytes/μl urine,
- approximately < 5 erytrocytes/field of view.
Epithelium
They come from the epithelial lining of the renal tubules and urinary tract.
- Renal tubular cells
- Their occurrence in urinary sediment is always a pathological finding and indicates serious kidney damage, especially for diseases affecting the tubules ( acute tubular necrosis , acute interstitial nephritis ). They are relatively small cells (average size 13 μm) only slightly larger than leukocytes, either round, irregularly polygonal, cubic or faceted with a smooth, usually eccentrically placed (dark blue in the colored sample) round nucleus, without nucleoli. They are characterized by a granular cytoplasm, red in the stained sample. They usually occur alone, sometimes in clusters or can form cylinders.
- In the unstained preparation, they are difficult to distinguish from transitional epithelial cells. Therefore, the term "small round epithelial cells" is sometimes used in laboratory practice. They can also be mistaken for leukocytes.
- Transient epithelial cells
- They come from the superficial or deeper layers of the transitional epithelium lining the urinary tract. It is not possible to locate them in a certain part of the urogenital tract. A more common finding is surface layer cells that are round or ovoid with a round or ovoid nucleus located centrally or slightly eccentrically with a visible nucleolus and a cytoplasm that is usually finely granulated (less than tubular cells), granulation is usually on the periphery of the cell, rarely around the core. The average size is around 30 μm. Their findings usually indicate an infection of the lower urinary tract, especially in the presence of leukocytes. They can also be found in the urine of healthy people.
- Cells from deeper layers are smaller (average size 17 μm), ovoid and their shape is much more variable (shape of clubs, hammers or cells with tails). Dual-nuclear cells are a common finding. We encounter them in the urine of patients with urothelial carcinomas or urinary stones .
- Squamous epithelium
- They are the largest cells in the urinary sediment (average size 55 μm), rectangular to polygonal in shape with a small nucleus and rich cytoplasm. They come mostly from the urethra or vagina and their amount depends on the quality of the urine sample. They are usually found in the urine of women when poorly contaminated, they have no diagnostic significance .
Tumor cells
- Tumor cells can be released into the urine in tumors of the kidneys, urinary tract and accessory organs (eg prostate). They are characterized by an irregular shape of the nucleus, which is usually significantly larger in relation to the cytoplasm. Without staining, the presence of tumor cells is difficult to detect (Table 3).
- Tab. 3 Basic morphological characteristics of urinary sediment cells
| Cell type | Kernel | Cytoplazma |
|---|---|---|
| Erythrocyte | bezjaderný element | discoid bodies |
| Granulocyt | segmented, multilobed, bright blue, sometimes poorly colored | granular, usually colored red |
| Macrophage | often broken blue nuclei, inhomogeneous chromatin | granular, usually contains parts of erythrocytes or other phagocytosed material |
| Lymphocyte | large, smooth nucleus, filling almost the entire cell | thin edge of cytoplasm without granulations |
| Tile cell | degenerate, small (polygonal) located in the middle | indistinctly rich |
| Superficial transitional epithelial cells | oval or round, usually deposited in the center of the cell, chromatin finely granulated, occasionally nucleolus occurs | finely granulated cytoplasm, granulation more often at the periphery of the cell |
| Transient epithelial cells deep | well defined, distinct nucleoli | numerous granules may be dark red |
| Renal tubular cell | homogeneous clear, spherical or oval, usually eccentrically arranged | the coarser granulated dense cytoplasm, often dark red, may contain fat particles inside |
Rollers
The cylinders are cylindrical structures formed in the distal tubules and collecting ducts of the kidneys. The matrix is made up of Tamm-Horsfall protein , which is produced by the tubular epithelial cells whose surface it protects. Under certain circumstances, such as low pH , high osmolality , high protein concentrations, Tamm-Horsfall protein can precipitate and form casts of tubules that are released into the urine. On microscopic examination, they are described as cylinders. During the precipitation, other material can be incorporated into the cylinder matrix, eg cellular elements (leukocytes, erythrocytes, renal cells), pigments (hemoglobin, bilirubin), crystals and plasma proteins. Cylinders are the only elements that are always of renal origin, cannot come from the urinary tract. The morphology of the cylinders depends on the diameter of the tubules in which they form. If the tubule in which the cylinder is formed is enlarged due to atrophy or obstruction, wide cylinders, typical of kidney failure, form .
According to their appearance, the cylinders are classified into:
- cellless
- hyalins,
- granular,
- waxy,
- fat;
- cellular (the area of the cylinder is more than 1/3 covered by cells)
- erythrocyte,
- leukocyte,
- epithelial,
- bacterial.
Demonstration of cell cylinders in urinary sediment is always a sign of a pathological process in the kidneys (Table 4).
- Tab. 4 Overview and diagnostic significance of individual types of cylinders in urinary sediment '
| Cylinder designation | Characteristics | Diagnostic significance |
|---|---|---|
| Hyalinní |
|
|
| Granulated |
|
|
| Wax |
|
|
| Grease and fat cell cylinders |
|
|
| Epithelial |
|
|
| Erythrocytes |
|
|
| Leukocytové (granulocytové) |
|
|
| Bacterial |
|
|
Microorganisms
- Under physiological circumstances, the urine contains bacteria in an amount of less than 10 5 / ml. They have the appearance of small coccal or rod-shaped formations, which differ from other elements.
- The presence of bacteria can also be a sign of non-sterile urine collection, as the bacteria multiply rapidly when the sample is allowed to stand for a long time.
- They have a round or oval shape with whips, they are characterized by fast irregular movement when alive. Their frequent finding is in concomitant inflammation of the vagina.
- They are slightly smaller than erythrocytes, oval but of various sizes. We find them in groups and sometimes grouped in the form of chains. They are common in diabetics, in patients treated with immunosuppressive drugs and sometimes after antibiotics.
Crystals
Examination of the crystals must be performed in the morning urine immediately after its collection. The finding of crystals, which occur relatively frequently in the urinary sediment, cannot be overestimated. The presence of crystals may be due to transient urinary supersaturation, eg when eating food rich in urates or oxalates, and is a signal for increased fluid intake. Crystals form in vitro as the urine sample cools or the pH changes. The finding of crystals in these circumstances is clinically insignificant.
- Uric acid crystals and amorphous urates in acidic urine and ammonium magnesium phosphate in alkaline urine in urinary tract infections are common .
- Crystal detection is important in patients with urolithiasis. Their ID can indicate what kind of stones it is. However, it is not possible to conclude from the findings of crystals in the urine that there is a concrete of the same chemical composition in the urinary tract. Repeated detection of crystals is especially important in the control of patients after removal of the stone or in patients with recurrence of urolithiasis.
- Identification of hexagonal cystine crystals will support the diagnosis of cystinuria.
- The finding of ammonium magnesium phosphate crystals together with high urine pH indicates the probability of struvite stones.
- Flooding of calcium oxalate crystals is a characteristic finding in ethylene glycol poisoning, otherwise these crystals are a common finding especially in people with a higher intake of plant foods and are not related to the formation of stones. Another example is uric acid crystals in urate nephropathy.
- The presence of leucine and tyrosine crystals accompanies severe liver disease. Also, some drugs may be excreted in the form of crystals, especially in overdose, dehydration or hypoalbuminemia. Urine pH also affects the nature of the drug.
- Cholesterol crystals are a sign of severe glomerular membrane damage (Table 5).
- Tab. 5 Selected crystals in urinary sediment
| Kind of crystal | Typical shape | Urine pH | Clinical significance | ||
| Sour | Alkaline | Variable | |||
| Urine | amorphous | + |
| ||
| Uric acid | various shapes, "kegs", "rosettes" | + |
| ||
| Ammonium urea | balls, "thorn apples" | + |
| ||
| Calcium carbonate | balls arranged in the shape of a dumbbell | + |
| ||
| Ammonium magnesium phosphate (triple phosphate) | coffin lid shape | + |
| ||
| Calcium oxalate | "Envelopes" (dihydrate), "biscuits" - (monohydrate) | + |
| ||
| Cholesterol | flat plates with broken corner | + |
| ||
| Cystin | hexagonal prisms | + |
| ||
| tyrosine | thin needles in bundles or rosettes | + |
| ||
| leucine | oily balls | + |
| ||
Lipids
- Lipids can enter the urine through the damaged glomerular membrane in the form of plasma lipoproteins. Lipoprotein particles are larger than the proteins themselves, and therefore lipiduria is associated with severe proteinuria and signals severe kidney damage.
- Lipids occur in the form of loose droplets isolated or in clusters; in this case, their presence may be caused by contamination, such as suppositories. Intracellularly localized fat inclusions are a sign of degenerative cell changes. Another form is cholesterol crystals or fat cylinders.
Other findings
- In the urinary sediment, we can also notice motile spermatozoa with a long thin flagellum, mucus and fibrin fibers and various contaminating formations, such as fibers of toilet paper or various textiles.
Quantitative examination of urinary sediment according to Hamburger
In indicated cases, a quantitative examination of urinary sediment according to Hamburger can be performed, which is used to monitor the rate at which erythrocytes, leukocytes and cylinders are excreted in the urine. The patient collects urine for 3 hours. As a last resort, a deviation of ± 30 minutes is tolerated, which must be taken into account in the calculation. At the end of the collection, the entire volume of collected urine is delivered to the laboratory within 1 hour. At the same time, it is necessary to state the collection time to the nearest minute. The number of erythrocytes, leukocytes and cylinders in the 5 large squares of the Bürker chamber is evaluated in the sediment.
- References values
- Erythrocytes up to 2000/min, ie. 33 Er/s.
- Leukocytes up to 4000/min, ie. 67 Leu/s.
- Cilinders up to 60–70/min, ie. 1 válec/s.
Automatic analysis of urinary sediment
Devices for automated examination of urinary sediment are currently available. They work on the principle of flow cytometry or digital particle sensing.
Flow cytometry
Flow cytometry is a laboratory method that allows the simultaneous measurement of a number of parameters in a large number of particles. In addition to hematology, its application in the examination of urinary sediment is gradually expanding, which has hitherto significantly burdened laboratories and, in addition, has been burdened with subjective error. In flow cytometry, the particles are labeled with different fluorophores and then the cell suspension is driven through a narrow capillary. As they pass through the capillary, the particles encounter a beam of light, usually from a laser, which excites the fluorescence of the fluorophores. The laser light is scattered by the cell. The most frequently measured parameters are light scattering at a small angle , which is directly proportional to the size of the cells - the so-called forward scatter, light scattering to a large angleso-called side scatter, which provides information about the internal structure of particles, and fluorescence of different wavelengths. The flow cytometer is a fully automated analyzer for the analysis and identification of cells and other elements of native urine samples.
- Analysis procedure
- When examining the urine sediment by flow cytometry, the urine is aspirated (0.8 ml) after mixing, diluted and the conductivity is measured.
- This is followed by automatic staining of the urinary elements with two different fluorescent dyes. The phenanthridine dye stains nucleic acids (orange fluorescence). The second dye used - carbocyanine is intended for staining of negatively charged cell membranes, nuclear membranes and mitochondria (green fluorescence).
- The colored particles pass through the capillary and are irradiated with a laser beam, which is both scattered by the cell and excited by the fluorescence of the fluorophores. At the same time, the electrical conductivity of the particles in the capillary is measured . Identification and counting of elements is made possible by evaluating the fluorescence of both dyes together with measuring the scattering of the radiation emitted by the laser and the measured conductivity.
All cell elements - erythrocytes , leukocytes , bacteria and epithelial cells - can be diagnosed using a flow cytometer . In addition, it is able to differentiate some clinically significant modifications such as isomorphic and dysmorphic erythrocytes . Provides information on the presence of pathological cylinders, which, however, need further microscopic examination. It also demonstrates crystalline structures, but does not distinguish between different types of crystals, in which case microscopic refinement is required. The flow cytometer is unable to differentiate trichomonads. The number of erythrocytes, leukocytes, bacteria, flat epithelium and cylinders is given in elements / μl. To increase the accuracy of urinary sediment analysis, it is possible to automatically compare the results of chemical analysis using diagnostic strips, which is evaluated by a reflection photometer, and analysis by flow cytometry, so-called cross-check. Conformity of flow cytometry with microscopy ranges from 80-90%, agreement with diagnostic strips in 72-96%. Flow cytometry significantly reduces the need for microscopic analyzes, improves measurement accuracy and facilitates standardization of results.
Digital particle sensing
In this method of automatic urine sediment analysis, a sample of uncentrifuged urine is injected into a planar cuvette. Particles present in the urine are scanned multiple times using a digital camera and their images are compared based on their size, shape and structure with a database that is part of the device software.
Urine test reference values
- Chemical examination
- pH 5–7.
- Relative density 1,016–1,022.
- Protein up to 0.3 g / l.
- Glucose negative.
- Ketone bodies negative.
- Bilirubin negative.
- Urobilinogen 3,2–16 μmol/l.
- Blood up to 5 / μl.
- Leukocytes up to 10 / μl.
- Nitrite negative.
- Sediment (quantitative)
- Erythrocytes <33 / s.
- Leukocytes <67 / s.
- Cylinders <1 / s, only hyaline.
Results of chemical examination of urine and urinary sediment in urinary tract infections
__
If a urinary tract infection is suspected, we examine the urine chemically and evaluate the urinary sediment, among other things. In indicated cases, we also use urine culture tests with evidence of antibiotic susceptibility.
Chemical examination of urine
In the chemical examination of urine , we can find a number of abnormalities in urinary tract infections:
Alkaliuria
Some bacteria (eg Pseudomonas , Klebsiella ) break down urea into ammonia by the enzyme urease. This alkalizes the urine. Therefore, we should always think about a urinary tract infection if the pH of the urine is higher than 6.5. However, more acidic urine does not rule out a urinary tract infection.
Nitrites
In particular, gram-negative bacteria (mainly E. coli , Proteus , Klebsiella , Aerobacter ) can reduce nitrates to nitrites. Nitrite detection is thus an indirect sign of bacteriuria. This test is very specific, but its sensitivity is only around 50%.
Hematuria
It is detectable in most urinary tract infections. The presence of peroxidases in bacteriuria can also cause a positive blood test for urine. Unfortunately, the test is not very specific.
Leukocyturia
It also accompanies a large proportion of urinary tract infections. Quantitative examination of urinary sediment is more sensitive than chemical examination of urine.
Proteinuria
The amount of protein in the urine in urinary tract infections varies from concentrations that cannot be determined by basic techniques to values around 2 g / l.
Other findings in chemical examination of urine
In urinary tract infections, false positives of bilirubin , urobilinogen and ketone bodies are often false .
It follows that the result of a chemical urine test can be very abundant in urinary tract infections. On the other hand, we also encounter bacteriuria with a completely normal chemical finding. Therefore, any combination of results between these two extremes is compatible with the diagnosis of urinary tract infection. However, the following applies:
- If there are positive nitrites, the urinary tract infection is almost certain (specificity> 95%). Quite often, however, in a urinary tract infection, nitrites remain negative (sensitivity around 50%).
- In 98% of urinary tract infections, at least one of the parameters of hematuria, leukocyturia, nitrites, proteinuria is positive . With the exception of nitrites, however, the finding is often caused by another cause and urinary tract infection must therefore be confirmed by further examination (microscopically and by culture).
Sediment examination
Higher erythrocyte and leukocyte counts are usually found in urinary sediment for urinary tract infections ; in these parameters, the sediment examination is more sensitive than the chemical examination. Furthermore, there are usually higher numbers of epithelial cells corresponding to the site of inflammation, and of course we find a larger number of bacteria .
Links
References
- HOHENBERGER, EF and H KIMLING. Compendium urinanalysis. Urinanalysis with test strip [online] . 1st edition. Mannheim: Roche Diagnostics, 2008. 105 pp. Also available from < http://www.diavant.info/diavant/servlet/MDBOutput?fileId=1392 >.
- ↑ PLIVA-Lachema Diagnostics. PHAN® diagnostic urine test strips [online]. Last revision 2009-12-04, [cit. 2010-03-21]. < https://www.erbalachema.com/cz/ >.
- ↑ PECKOVÁ, Marie. Basic sets of laboratory tests: Chemical, microscopic and bacteriological examination of urine [online]. © 2011. [feeling. 2014-05-27]. < http://www.propedeutika.cz/met_lab_moc.html >.
- ↑ FOX, Gary N. Sensitivity and specificity of urinary nitrite for UTIs. Am Fam Physician [online]. 2005, vol. 72, no. 11, s. 2180; author reply 2180, 2182, dostupné také z <https://www.ncbi.nlm.nih.gov/pubmed/16342841>. ISSN 0002-838X.
- ↑ PATEL, H D, S A LIVSEY a R A SWANN, et al. Can urine dipstick testing for urinary tract infection at point of care reduce laboratory workload?. J Clin Pathol [online]. 2005, vol. 58, no. 9, s. 951-4, dostupné také z <https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1770822/?tool=pubmed>. ISSN 0021-9746.
- https://www.wikiskripta.eu/w/Vy%C5%A1et%C5%99en%C3%AD_mo%C4%8Di
External links
- DASTYCH, Milan and Jaroslav WINKLER. Automated urinalysis [online]. Portal of the Faculty of Medicine of Masaryk University, ©2005. Last revision 2011-10-27, [cit. 2011-11-25]. < http://portal.med.muni.cz/clanek-10-automaticka-analyza-moci.html >.
References
- SCHNEIDERKA, Petr, et al. Chapters in clinical biochemistry. 2nd edition. Prague: Karolinum, 2004. 365 pp. ISBN 80-246-0678-X .



![{\displaystyle \mathrm {H} _{2}\mathrm {O} _{2}+\mathrm {H} _{2}\mathrm {A} \ {\xrightarrow[{\mathrm {nebo\ hemoglobin\ a\ jin{\acute {e}}\ l{\acute {a}}tky} }]{\mathrm {peroxid{\acute {a}}zy} }}\ 2\ \mathrm {H} _{2}\mathrm {O} +\mathrm {A} }](https://wikimedia.org/api/rest_v1/media/math/render/svg/23377fd4d265df004d50c7657f43bcbbe4cdc8ff)