Tracheostomy
Tracheostomy is a condition after a surgical procedure - tracheotomy, when the trachea is artificially opened to the surface of the body. The aim is to ensure patency of the airways to enable ventilation (spontaneous or with the help of a device). It can be permanent (eg after total laryngectomy) or temporary.
Options for invasive airway management[edit | edit source]
- endotracheal intubation – oral, nasal ,
- ostomy – laryngostomy, tracheostomy .
- Tracheostomy (artificial connection of the trachea to the surface of the body) - arises from:
- tracheotomy – cutting the wall of the trachea,
- tracheopuncture – puncture of the trachea.
- Laryngostomy (artificial connection of the larynx to the surface of the body) - arises from
- coniotomy – cutting lig. conicum(membrana cricothyroidea), a method of emergency securing of the airways and is replaced by a tracheostomy as quickly as possible,
- coniopuncture – puncture through the lig. cone.
In the case of the need for acute airway management, endotracheal intubation is the method of choice , if this is not possible, coniotomy or coniopuncture is performed, tracheostomy is performed only afterwards, if there are indications for it.
Indications for tracheostomy[edit | edit source]
- Airway obstruction – tumors, congenital anomalies, severe traumas devastate the face, post-operative conditions – ENT and stomatological surgeries, sleep apnea syndrome, paresis of the vocal cords, foreigh bodies in the larynx, tracheomalacia,
- long term artificial lung ventilation ,
- securing the airways without the need for ventilation support – disorders of consciousness In patients with the need for long-term introduction of orotracheal intubation, tracheostomy is usually performed between the 2nd and 10th day (the patient is intubated before that, most often on the 7th-10th day), when there is a risk of damage to the vocal cord muscles and ligaments due to atrophy during intubation. In the case of certainty of long-term UPV, the earlier the better rule usually applies , but studies have shown that in some patients with a delayed tracheostomy date (after the 10th day), conversion was not needed as a result and the patient was successfully extubated.
Tracheostomy vs. intubation[edit | edit source]
The work of breathing jis less when converting to a tracheostomy, thus allowing better parameters for UPV weaning, and the synchronization of one's own breaths with the ventilator can also be improved. Compared to the use of an intubation cannula, there is less anatomical dead space with a tracheostomy, which reduces the work of breathing and makes it easier for the patient to trigger ventilation support during assisted breaths.
The risk of aspiration during long-term ventilation is similar for both methods (accumulation of secretions above the sealing balloon). Based on the available data, it is not possible to determine exactly whether any of the methods increases the risk of ventilator-associated pneumonia .
Communication with the patient, patient comfort and weaning sedation options jare better addressed in patients with a tracheostomy. For patients, tracheostomy is usually more pleasant, they tolerate it much better, it allows full muting and some communication, some types of tracheostomy tubes also allow articulate speech. The cannula also allows for oral intake of food, is easier to fix and has less risk of dislocation.
The disadvantages of tracheostomy are associated with the risks of surgery, as well as with a negative cosmetic effect, loss of function of the nasal cavity and changes in breathing mechanics by removing part of the dead space.
Basic methods[edit | edit source]
- Surgical tracheostomy (upper, middle, lower - according to the height of the transection of the trachea relative to the isthmus of the thyroid gland).
- Puncture dilatation tracheostomy (PDT) – modification of the Seldinger technique.
Method selection[edit | edit source]
Today's research shows that puncture dilatation tracheostomy has advantages over surgery in most cases . It has a lower frequency of infectious complications, less bleeding, and according to some studies, it also reduces scarring. The performance takes less time and is cheaper.
Relative contraindications to PDT leading to a preference for a surgical approach include uncorrected hemorrhagic diathesis (performance usually bleeds less, but with complications, bleeding is more difficult to stop), age under 15 years, large neck hematoma causing anatomical disproportion, soft tissue infections of the neck, instability of the cervical spine, obesity and other conditions worsening the anatomical clarity of the terrain.
Another disadvantage is the greater risk of injury to the back wall of the trachea and its rings. Furthermore, in the first days after insertion, the opening in the trachea closes very quickly during dislocation, which makes it impossible to reposition it. In case of early dislocation of the cannula after PDT, the staff must not attempt manual reduction! This procedure usually leads to the introduction of a cannula into the upper mediastinum due to the already closed opening in the wall of the trachea and the creation of a pneumomediastinum
Surgical tracheostomy[edit | edit source]
- The skin incision
- is 6 to 8 cm long and can be:
- horizontal - more common, according to the lines of skin cleavage - in the middle of the distance between the lower edge of the annular cartilage and the upper edge of the sternum,
- is 6 to 8 cm long and can be:
- The next procedure is the same for both horizontal and vertical cuts:
- vertical – in the midline between the lower edge of the annular cartilage and the jugular. The next procedure is the same for both horizontal and vertical cuts:
- intersection of the platysma muscle and the surface sheet of the cervical fascia,
- we get to the infrahyoid muscles , which are wrapped in the middle sheet of the cervical fascia, strengthened in the midline in the linea alba colli - we cross this vertically and move the infrahyoid muscles to the sides,
- we penetrate to the capsule of the thyroid gland and release its isthmus (disruption of the fascia laryngothyroidea – fibrous connection between the capsule of the thyroid gland and the annular cartilage), the isthmus is then dissected from the front wall of the trachea,
- the isthmus is then cut off and its stumps are caught by opihs,
- incision of the anterior wall of the trachea (general rules – we never cut the 1st tracheal ring, we never cut more than 2 tracheal rings):
- window by cutting out the front wall of the 2nd or 3rd ring,
- U-lobe, H-cut, T-cut,
- 6. followed by insertion of a tracheostomy cannula and suturing of the wound.
- Anatomical structures that can get in the way of a tracheotomy
- Upper tracheostomy:
- lobus pyramidalis glandulae thyroideae.
- Lower tracheostomy:
- arcus venosus juguli (vv. jugulares anteriores) in the spatium suprasternale ,
- plexus thyroideus impar (vv. thyroideae inferiores) in spatium praeviscerale ,
- a. thyroidea ima in the spatium praeviscerale, behind the plexus venosus impar ,
- large vessels coming from the apertura thoracis superior (especially in children, where they are placed higher) .
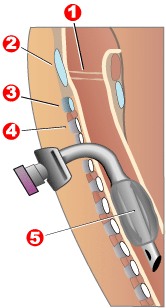
Puncture dilatation tracheostomy[edit | edit source]
It is usually carried out under endoscopic control and possibly with an ultrasound examination to clarify the anatomical structures and prevent mainly bleeding complications. The principle is a puncture of the trachea wit ha special needle, after removal of the stylet, a wire is inserted through it, the needle is removed and dilators of increasing diameter are gradually introduced after the wire, or the channel is dilated with special dilatation forceps. Finally, the cannula is inserted and the wire is removed. There are a number of other, modified techniques.
Complications of tracheostomy[edit | edit source]
- Intraoperative:
- bleeding , trachea or larynx injury , air embolism ,
- pneumothorax , pneumomediastinum,
- respiratory insufficiency (bleeding into the airways, dislocation or obstruction of the tracheal tube, bronchospasm),
- incorrect insertion of the puncture needle in PDT,
- paratracheal tube insertion,
- injury to recurrent laryngeal nerve or thyroid gland,
- incorrect size of the window during surgical access (small - bruises, impossibility of insertion; large - late stenosis of the trachea).
- Postoperative:
- tracheostomy tube dislocation,
- infection around the tracheostomy, respiratory tract infection,
- subcutaneous, mediastinal emphysema ,
- respiratory insufficiency ,
- pressure ulcer from cannula pressure,
- tracheoesophageal fistula,
- tracheomalacia .
- After decannulation:
- decannulation panic (a feeling of shortness of breath due to a sudden increase in dead space),
- dysphagia , dysphonia , aspiration ,
- stenoses (subglottic, trachea at or below the tracheostomy site),
- tracheocutaneous fistula.
Links[edit | edit source]
Related articles[edit | edit source]
External links[edit | edit source]
References[edit | edit source]
- ŠEVČÍK, Pavel, et al. Intenzivní medicína. 3. edition. Galén, 2014. 1195 pp. pp. 74–78. ISBN 978-80-7492-066-0.
- HYZY, Robert C, et al. Overview of tracheostomy [online]. UpToDate, The last revision 2020-04-16, [cit. 2020-05-19]. <https://www.uptodate.com/contents/overview-of-tracheostomy>.
- PASTOR,. Langenbeck's medical web page [online]. ©-. [cit. 2009-11-23]. <http://langenbeck.webs.com>.