Silicosis
Silicosis in lung damage (mostly occupational) caused by inhalation of inorganic material – in this case fibrogenic particles of silicone dioxide SiO2.
Silicosis:
Etiology[edit | edit source]
Characteristics of noxy[edit | edit source]
- SiO2 is the main component of earth minerals, it occurs:
- free (not fibrogenic) – in three main forms – crystalline, cryptocrystalline and amorphous,
- modification of the crystalline form – quartz, tridymite and cristobalite (the least fibrogenic quartz),
- bound in compounds such as silicates.
Professional exposure[edit | edit source]
- Wherever rocks with quartz (granite, sandstone, slate) are separated and processed,
- mainly – underground miners, tunnelers,stone breakers and miners,
- in foundries – sandblasters, foundries, quartz sand blasters,
- stoneware (marble and limestone are not fibroproductive),
- white masons (clay bricks), workers in the ceramic industry.
- dental technicians in small quantities when processing ceramics, glass ceramics and zirconium as well as when sandblasting metal alloys and zirconium
Etiopathogenesis[edit | edit source]
The mechanism of the disease is not fully understood. Respiratory SiO2 (0,6–5,0 µm in size), that reach the lung interstitium and lymph nodes (most of them are coughed up or swallowed) activate lung macrophages for phagocytosis and the release of pro-inflammatory cytokines, fibroblast growth factors (proliferation stimulation fibroblasts and collagen formation), IL-1 and leukotriene B4 (chemotactic factor for neutrophils).
Silicosis can be combined with soot dusting (anthracosilicosis = coal mine disease) or iron particles (siderosilicosis), previously it was often combined with tuberculosis (tuberculosilicosis).
Pathological findings in silicosis[edit | edit source]
Macroscopy[edit | edit source]
Characteristic are silicotic nodules (mainly around the respiratory bronchioles, perivascularly, subpleurally). On a section of the lung, we see solid gray nodules (2-6 mm in diameter). Nodules can deposit calcium (shotgun lung on X-ray), or cluster into larger nodules. Hilar and paratracheal nodes are enlarged, fixed (they often form dilatation of the trachea and bronchi). Sometimes they also calcify under the capsule („shell node“). The fibrotic visceral pleura often fuses with the parietal pleura. The upper lobes of the lungs are particularly affected.
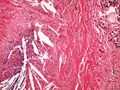
Microscopy[edit | edit source]
The basis is a cluster of macrophages with SiO 2 particles in the cytoplasm, concentrically arranged collagen fibers are formed in the center, parts turn into acellular hyaline surrounded by a bulbous layered collagen capsule.
Stages of silicosis[edit | edit source]
Dusting takes place in three stages:
- stadium – mild diffuse reticular fibrosis,
- stadium – the formation of silicotic nodules the size of a millet, they are formed by concentrically layered hyalinized tissue, there may be necrosis in the center, perifocal emphysema around the nodules, sometimes they have a scalloped contour,
- stadium – compact fibrosis with coalescence of silicotic nodules.
Investigation methods[edit | edit source]
- X-ray of chest – small nodules up to 10 mm are typical for simple nodular silicosis, larger fibrotic deposits for complicated silicosis, enlargement of the hilar nodes (shell pattern), often also dislocation of the trachea and bronchi, in acute cases there may be obscuration of the lower lung fields or findings resemble miliary tuberculosis,
- HRCT for fine interstitial lesions,
- examination of lung functions (spirometry) – in simple silicosis the values are usually within the norm, but primarily obstructive disorders will appear, or combined disorders (obstruction+restriction), X-ray findings may not correlate with spirometry and subjective description of difficulties
- BAL – certificate of particles.
Types of disease[edit | edit source]
Chronic silicosis[edit | edit source]
It occurs after exposure for more than 10 years. It is divided into simple and complicated silicosis:
Simple silicosis[edit | edit source]
It can be completely asymptomatic for a long time, symptoms (cough, expectoration) often develop very slowly.
- X-ray findings – bilateral dissemination of small nodules, mostly in the upper lung lobes, enlargement of the lung hilae with shell-like calcifications (nodules).
Complicated silicosis[edit | edit source]
It is caused by the progression of simple silicosis, the symptoms worsen.
- Symptoms:
- cough and expectoration - almost always,
- exertional dyspnea – in more advanced stages, rest dyspnea also develops,
- cyanosis – in the last stages of the disease,
- club fingers – rarely,
- respiratory insufficiency.
- X-ray finding – the appearance of large fibrotic nodes or areas of massive fibrosis, which were formed by fusion, compensatory emphysema develops in the remaining parenchyma.
- Complications of the disease:
- the disease is sometimes associated with pulmonary tuberculosis or other mycobacteriosis,
- development of pulmonary hypertension, cor pulmonale, heart failure.
Subacute (accelerated) silicosis[edit | edit source]
It occurs after a shorter, more intense exposure (2–5 years), the picture of this form corresponds to simple nodular silicosis.
Acute silicosis[edit | edit source]
Overall, very rare, it arises after several months of very intensive exposure. It practically does not occur in our conditions. Symptoms usually disappear quickly (rapidly progressing shortness of breath, cough, fatigue, weight loss).
Complication[edit | edit source]
- COPDS,
- bronchogenic carcinoma – silicosis is RF for formation (SiO2 is in IARC group 1),
- pulmonary hypertension, cor pulmonale chronicum, heart failure,
- perifocal (pericicatric) emphysema,
- bronchiectasis.
Differential diagnosis[edit | edit source]
- Other disseminated pulmonary processes such as sarcoidosis and tubercolosis,
- cryptogenic and exogenous fibrosis alveolitis,
- acute bronchiolitis,
- lung metastases,
- histiocytosis X.
Therapy[edit | edit source]
There is no causal treatment, we limit ourselves to symptomatic treatment, therapy of complications
- bronchodilation in obstructive dyspnea ,
- oxygen therapy ,
- antibiotics in the treatment of infections,
- lung transplantation.
Despite all measures, silicosis is an unstoppably progressive disease.
Assessment of professionalism[edit | edit source]
- X-ray evaluation according to the ILO (International Labor Organization) International Classification of pneumoconioses,
- designation of nodules – „p“ (up to 1,5 mm), „q“ (1,5–3 mm), „r“ (3–10 mm),
- designation of nodes – „A“ (one deposit 10–50 mm, or several deposits over 10 mm, the sum of which does not exceed 50), „B“ (more than A, not exceeding the right upper lung field in total), „C“ (exceeds the equivalent upper right field),
- frequency desgination – 1, 2, 3,
- as occupational diseases we consider p3, q2, q3, r2, r3 and all complicated ones (A, B, C), "ones" (p1, q1, r1 and above) are sufficient in connection with tuberculosis, we further describe the so-called dynamic form, which occurs in individuals under the age of 40 who have no exceeded 15 years (3000 shifts) at risk of exposure and yet have at least p2, q1, r1 and above.
Links[edit | edit source]
Related articles[edit | edit source]
Source[edit | edit source]
- BENEŠ, Jiří. Study materials [online]. [cit. 24.02.2010]. <http://jirben.wz.cz>.
Recommended literature[edit | edit source]
- PELCLOVÁ, Daniela. Nemoci z povolání a intoxikace. 2. edition. Karolinum, 2006. 207 pp. ISBN 80-246-1183-X.
- ČEŠKA, Richard. Interna. 1. edition. Triton, 2010. 855 pp. pp. 494-495. ISBN 978-80-7387-423-0.
- PASTOR,. Langenbeck´s medical web page [online]. ©2005. [cit. 2011-03-26]. <https://langenbeck.webs.com/>.