SINGLE-PHOTON EMISSION COMPUTED TOMOGRAPHY (SPECT)
- Previous chapter: 6.4 COMPUTED TOMOGRAPHY (CT)
Single-photon emission computed tomography (SPECT, or less commonly, SPET) is a nuclear medicine tomographic imaging technique which uses a source of gamma rays which are emitted from the source and pass through the body. Similar to the gamma camera it is capable of producing true 3D images. These images are usually obtained as cross-sectional slices through the patient.
The first order of operation is to produce such gamma rays. The source of it is a radionuclide active material which is applied into the patient’s body, usually into the bloodstream. There are many radionuclides used but the most commonly used are Tc99m (technetium-99m) or I123 (iodine 123). This applied solution is then distributed all over the body, including the investigated part.
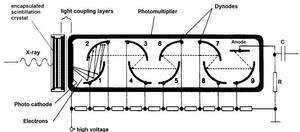
Since the high energy gamma rays are invisible to the human eye, we usually produce the images with the aid of scintillators. Scintillators are devices that are able to acquire x-ray or gamma photons for next processing. These scintillators consist of a scintillation crystal and a photomultiplier tube (PMT).
High energy X-rays or gamma rays reach the scintillation crystal. Part of their energy is absorbed and the rest is emited as lower energy photons, usually in the visible spectrum. However, this emission doesn't produce a significant amount of photons.
These converted photons have to be somehow detected. For this we use PMT tubes, which are vacuum tubes. These are extremely sensitive detectors of light in the ultraviolet, visible, and near-infrared ranges of the electromagnetic spectrum. These detectors multiply the current produced by incident light by as much as 100 million times, in multiple dynode stages, enabling individual photons to be detected when the incident flux of light is very low.
The visible light (or UV, near IR) photon reaches the photocathode. Because of the photoelectric effect electrons produced. These electrons are accelerated through dynodes stages where their count is multiplied by a secondary emission effect. The acceleration is caused by high voltage that is applied. Then the value can be obtained by simple voltmeter where the voltage represents light intensity.
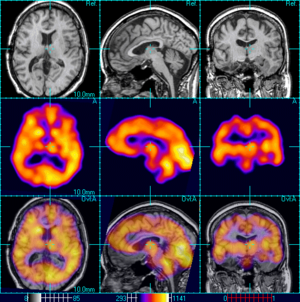
In the same way that a plain X-ray is a 2-dimensional (2-D) view of a 3-dimensional structure, the image obtained by a gamma camera is a 2-D view of 3-D distribution of a radionuclide. SPECT imaging is performed by the use of a gamma camera in order to acquire multiple 2-D images (also called projections) from multiple angles. A computer is then used to apply a tomographic reconstruction algorithm to the multiple projections, yielding a 3-D dataset. This dataset may then be manipulated to show thin slices along any chosen axis of the body, similar to those obtained from other tomographic techniques, such as MRI, CT, and PET.
To acquire SPECT images, the gamma camera is rotated around the patient. Projections are acquired at defined points during the rotation, typically every 3–6 degrees. In most cases, a full 360-degree rotation is used to obtain an optimal reconstruction. The time taken to obtain each projection is also variable, but 15–20 seconds is typical. This gives a total scan time of 15–20 minutes.
SPECT can be used to complement any gamma imaging study, where a true 3D representation can be helpful, e.g., tumor imaging, infection (leukocyte) imaging, thyroid imaging or bone scintigraphy
Because SPECT permits accurate localisation in 3D space, it can be used to provide information about localised function in internal organs, such as functional cardiac or brain imaging.
Links[edit | edit source]
Bibliography
NAVRÁTIL, Leoš a Jozef ROSINA, et al. Medicínská biofyzika. 1. vydání. Praha : Grada, 2005. 524 s. s. 435. ISBN 978-80-247-1152-4.
KUPKA, Karel, Jozef KUBINYI a Martin ŠÁMAL, et al. Nukleární medicína. 1. vydání. vydavatel, 2007. 185 s. s. 49-53. ISBN 978-80-903584-9-2.
Next chapter: 6.6 POSITRON EMISSION TOMOGRAPHY (PET)
Back to Contents