Polytrauma
Polytrauma is the involvement of at least two organ systems, at least one of which threatens the patient's life .
A combined injury is an impairment of at least two organ systems that do not threaten the patient's life.
Epidemiology[edit | edit source]
Polytraumas are the most common cause of death under the age of 40, the incidence of trauma-related deaths in developed countries is 60-80/100,000 population, it is the fifth most common cause of death, the most common cause is traffic accidents.
Distribution of deaths[edit | edit source]
- Immediate - 50% during the first 30 min. – serious injuries to the brain , spine, heart or large vessels.
- Early - 30% in the first 4 hours - DC obstruction, insufficient ventilation, hemo - pneumothorax .
- Late - 20% ARDS, MOF, sepsis, pulmonary embolism .
Mechanism of injury[edit | edit source]
- High speed vehicle collisions.
- Fall from more than 4 meters.
- Explosion.
- Backfilling.
Typical injury mechanisms cause typical injuries:
- frontal impact – direct injury to the head, cervical spine, lower limbs, pelvis and chest;
- fall from a height – lower limb fractures, skull base fractures, trauma to the spine, pelvis, injuries to internal organs;
- blast – chest, limb, abdominal trauma, blast syndrome – pressure wave injury;
- crushing – crush syndrome, damage to internal organs.
Polytrauma surgical scoring[edit | edit source]
- Abbreviated Injury Scale = AIS
Individual injuries are evaluated according to the degree of severity from 1 to 6 - from the lightest 1 to the most severe (inoperable) 6.
- Injury Severity Score = ISS
Individual injuries are graded according to the AIS scale - and divided into six areas (head, face, chest, abdomen, limbs including pelvis, external injuries) - only the highest AIS value in the given region is counted. The ISS takes on values from 0 to 75. If a region in the AIS is rated as grade 6 (inoperable), the ISS automatically takes on the value of 75.
Rupture of the spleen
2
5
Management of care for the polytraumatized patient[edit | edit source]
Caring for a polytraumatized patient usually begins with the treatment and transport of a polytraumatized patient by an RLP doctor (Rapid Medical Aid – a type of medical emergency service crew whose member is a doctor). It is important to set priorities and maintain calm and balance.
EMS doctors (medical emergency service)[edit | edit source]
Upon arrival at the scene - determination of the number of injuries, evaluation of the severity of injuries, stopping life-threatening bleeding, ensuring airways, securing venous access, pharmacotherapy, volume therapy, transport to a trauma center or an appropriate medical facility.
Algorithm[edit | edit source]
- A – Airway – ensuring patency of airways (!Watch out for spinal trauma).
- B – Breathing – assessment of breathing, frequency, sight, palpation, listening (chest injury, tracheal deviation, pneumothorax) and the resulting measures – mask breathing, chest puncture, etc.
- C - Circulation - Palpation of the pulse - if it is not palpable, we start immediate resuscitation, if the pulse is palpable, we measure the pulse, pressure - procedures - stop the bleeding, ensure venous access, replenish the volume, take blood for KO, HTK.
- D – Disability – indicative neurological examination – head trauma, pupil size, state of consciousness GCS .
- E – Examination – Orientation examination of other body systems – chest, abdomen, limbs.
- T – thermal management, transport and documentation. [2]
Hospital phase[edit | edit source]
Structure of the ATLS (Advanced Trauma Live Support) trauma protocol[edit | edit source]
- Short overall evaluation
- rough orientation, medical history.
- Primary evaluation
- A, B, C, D, E – possible resuscitation, then:
- Disarmament, venous access 2 cannulas at least 14G, BP, TF, saturation.
- Secondary evaluation follows stabilization of vital functions.
- Clinical examination, X-ray, chest drainage, CVK, urinary catheter, ultrasound of the abdomen, CT of the spine and skull, arterial access , CT of the head.
- Definitive treatment.
Treatment of serious injuries[edit | edit source]
- Urgent income + life-saving services.
- The first diagnostic phase within 30 minutes.
- Injury stabilization and stabilizing surgery 2-3 hours (necessary to stabilize the patient).
- Second diagnostic phase + definitive stabilization 7.–10. day.
- Delayed performance and recovery
Composition of the trauma team[edit | edit source]
- Traumatologist
- Anesthesiologist, intensivist
- Surgeon
- Radiographer
- Neurosurgeon, neurologist, orthopedist, ENT, urologist, oral and maxillofacial surgeon...
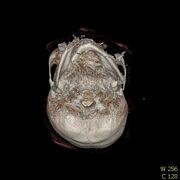
Reconstruction from CT skull polytrauma[edit | edit source]
Links[edit | edit source]
Related Articles[edit | edit source]
External links[edit | edit source]
- Polytrauma-MUNI Brno
- Doporučené postupy pro ošetření pacienta se závažným traumatem v přednemocniční péči