Periproctal fistula
A periproctal fistula is a pathological connection between the skin of the perineum and the rectum or anal canal. It occurs 8 times more often in men than in women. The overall prevalence is about 7/100,000 people. The average age is 40 years.
Etiology[edit | edit source]
There are also fistulas in the area of the rectum and perineum, which may not be related to the anus (from the female genitalia, urethra, prostate). Those that arise from the anal region and rectum can be divided into congenital and acquired.
- Congenital fistulas – they are part of the anomalies of the development of the anus.
- Acquired fistulas :
- – 80-90% arise on the basis of periproctal abscesses caused by anal gland infections (the so-called cryptoglandular theory).
- – 10-20% have another etiology: dermoid cyst , perineal trauma, Crohn's disease , pelvic inflammatory disease, TBC , cancers, radiation treatment, actinomycosis , chlamydial infection, or other sexually transmitted diseases .
- Rarer fistulas – horseshoe fistulas have long secondary trunks surrounding the anal canal, and are most often transsphincteric. If not recognized, it often recurs.
Division[edit | edit source]
Fistulas can be divided according to their relationship to the rectum - into rectal and periproctal (perianal). We further divide them into complete and incomplete according to whether they have an external and an internal mouth (complete) or only one (incomplete, more often external). A complex (complicated) fistula is one whose internal mouth extends above the puborectal muscle or its tract encircles more than 3/4 of the external sphincter.
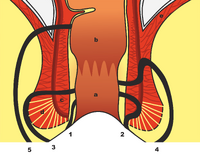
According to the anatomical location of the tract, fistulas are divided into:
- intrasphincteric (subcutaneous, submucosal),
- intersphincteric,
- transsphincteric,
- extrasphincteric.
According to Parks (intrasphincteric, transsphincteric, suprasphincteric, extrasphincteric).
Symptoms[edit | edit source]
Fistulas are manifested by secretion , itching and wetting of the surrounding area, soiling of laundry with feces or pus. The pain arises when the content stagnates when the drainage stops. Swelling and bleeding , feelings of fullness and pressure in the anus may also occur . Subfebrile states may also occur . Alternation of asymptomatic periods with symptomatic ones at intervals of varying lengths is common. An internal fistula may not manifest clinically at all.
Diagnosis[edit | edit source]
A thorough anamnesis with a focus on inflammation of the anorectum and abscesses in this area in the past, searching for symptoms of Crohn's disease is important . The physical examination is of greatest importance:
- Aspect - we find the external mouth of the fistula. Fistulas can have multiple external openings, but usually have only one internal opening. The distance from the anus can tell us what type of fistula it is. Closer to the anus - rather subcutaneous, further from the anus - more complicated fistulas.
- Goodsall's rule - if we draw an anem transverse line , then fistulas whose external mouth is dorsal to this line lead in an arcuate manner and have an internal mouth at No. 6 (middle posterior line). Fistulas that have an external mouth ventrally run straight and open radially at approximately the same position. However, Goodsall's rule does not apply 100%, there are more deviations in women.
- Palpation - by palpation you can detect a stiffer band, induration in the surrounding area. During a per rectal examination , we can sometimes feel the inner mouth as well.
- Anoscopy, rectoscopy, colonoscopy - allows to assess the mucous membrane of the rectum, the location of the internal oral fistula, exclusion of tumor or non-specific intestinal inflammation.
- Probing of the fistula - with a stick-shaped probe, we non-violently determine the course of the fistula, in case of great pain, it is performed intraoperatively under anesthesia. If the inner mouth is unclear, we can use a solution of hydrogen peroxide, betadine or methylene blue.
- Fistulography - contrast material is used for fistulas in Crohn's disease, recurrences or complicated course. This will show the branching, progress and blind trunks. However, the yield of the examination is low.
- US – endosonographic examination has recently been widely used and replaces CT examination, which is not very profitable for diagnosis. US can be used for primary diagnosis as well as intraoperatively.
- NMR - nuclear magnetic resonance is the most accurate method for imaging complicated fistulas , especially in Crohn's disease.
Treatment[edit | edit source]
The history of fistula treatment goes back to ancient times . Even then, Hippocrates used methods similar to today's, passing horse hair through fistulas (seton) and weighting the line with stones (cutting seton). The first comprehensive treatise on this issue comes from the 14th century (J. Ardern) and the fistulas did not escape even the French king Louis XIV.
Conservative techniques:
- Previously, conservative therapy with the application of sclerosing agents (eg AgNO 3 ) was widely used, but due to poor results, it is no longer used.
- Various fibrin tissue glues are used today , the most successful in treatment are tissue glues with intraadhesive ATB (other – autologous tl, tl without ATB).
Operating techniques:
- Fistulotomy, fistulectomy (lay open) - these similar procedures are performed for simple low fistulas without a complicated course. After clarifying the tract and the inner mouth, a grooved probe is introduced into the fistula and the fistula is dissected, the surrounding tissue is excised and the base is excochleated , and a tissue sample can be taken for histology. The wound is allowed to heal secondarly , or marsupialization is performed . In fistulectomy, excision is performed on the probe. With these techniques, however, there is a greater tissue defect and a greater percentage of postoperative incontinence . There are therefore various modifications of operations with preservation of the integrity of the external sphincter (Parks fistulectomy).
- Seton technique - (Hippocratic elastic ligature, cutting seton) is a technique used for higher transsphincteric, extra- and suprasphincteric fistulae. After identification of the external and internal mouth, a non- absorbable , preferably elastic fiber (silicone, rubber) is passed through the fistula and knotted under slight tension. The thread is gradually cut through the sphincter, it must be tightened to maintain approximately the same tension. Healing takes optimally 6-8 weeks, fibrotic tissue gradually forms behind the cut fiber . In a modification, the technique can be guided by the subcutaneous tissue. Indications must be considered, there is a greater risk of incontinence in women with ventral fistulae.
- Seton drainage is used for complex, multiple fistulas and fistulas in Crohn's disease . This technique is similar, but the fiber is introduced through the fistula freely without traction . In this way, non-elastic materials can also be used. Thanks to Seton drainage, the fistula gradually matures, followed by its excision . In Crohn's disease, tracing ligatures are used for long-term (weeks to months) drainage of fistulas with abscesses.
- Mucosal advancement flap – has the best results, can be used for almost all types of fistulas, is advantageous for complicated fistulas. Healing takes place advantageously per primam . Does not cause anal deformation. The method consists in fistulectomy from the outside of the sphincters, excision of the internal mouth, which is followed by the construction of a sliding mucosal flap , which is pulled into the defect and fixed with sutures around the perimeter. The external defect is left to secondary healing.
- Anal fistula plug – the use of special biological anal plugs that allow the fistula to heal.
New operating techniques:
- LIFT – Ligation of the Intersphincteric Fistula Tract – a new, relatively simpler technique of intersphincteric ligation.
- VAAFT – Video Assisted Anal Fistula Treatment – endoscopic examination of the fistula tract (fistuloscopy) with visualization of branching and the possibility of treatment of the inner mouth using a stapler or cutter.
- Fistula coagulation using RFA or laser.
Links[edit | edit source]
Related articles[edit | edit source]
Sources[edit | edit source]
- LADISLAV, Horák. Praktická proktologie. 1. edition. Praha. 2013. ISBN 978-80-247-3595-5.
- STANISLAV, Rejchrt. , et al. Přístup k paciento s píštělemi gastrointestinálního traktu. Folia Gastroenterologica et Hepatologica [online]. 2007, y. 5, vol. 5, no. 1, p. 19-29, Available from <http://www.pro-folia.org/files/1/2007/1/rejchrt.pdf>.
- PETR, Bartoška, et al. Perianální píštělě [online]. ZdravíE15, ©2007. [cit. 2014-04-01]. <https://web.archive.org/web/20160331222721/http://zdravi.e15.cz/clanek/postgradualni-medicina/perianalni-pistele-319038>.