Neutropenia in children
Neutropenia is defined as a decrease in the absolute number of neutrophils: total leukocyte count × (% neutrophils + rods) > 2 standard deviations from the mean value for age. From a clinical point of view, we distinguish between mild neutropenia (absolute neutrophil count 1000–1500/μl), moderate neutropenia (500–1000/μl) and severe neutropenia (< 500/μl). In children aged 14 days to 1 year, the limit values are lower (1000/μl is the lower limit of the norm). [1]
Neutropenia is a common finding in children. Etiology:
- infectious – transient neutropenia during a viral or a bacterial infection
- oncological
- autoimmune
- hereditary
Proliferation and maturation of neutrophil granulocytes[edit | edit source]
- takes place in the bone marrow, lasts 8-14 days
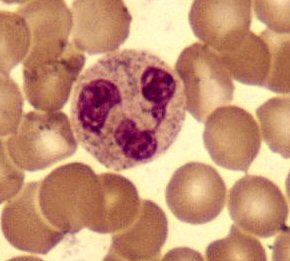
- proliferation (mitotic phase): myeloblasts → promyelocytes → myelocytes →
- maturation (postmitotic phase): → metamyelocytes → rods (both capable of phagocytosis)
Mature neutrophil granulocytes are constantly released into the peripheral blood (1-2×109 cells/kg/day). They live for 6-8 hours in the blood and 1-2 days in tissues. Polymorphonuclear cells in the blood are partly circulating and partly marginal (these adhere to the vascular endothelium using integrin molecules).
The accelerated release of neutrophil granulocytes from the bone marrow into the circulation (leukocytosis - neutrophilia) adrenaline and noradrenaline, complement fragments (C3e, C3d), stress hormones and infections. Inflammation (endotoxin) also stimulates G-CSF (granulocyte colony-stimulating factor), which prolongs the life and function of neutrophils. [1]
Role of neutrophil granulocytes[edit | edit source]
Neutrophil granulocytes (microphages, polymorphonuclear cells, neutrophils) play a central role in the inflammatory response. They mature in the bone marrow, from where they are released into the blood and tissues, where they act as the host's first line of defence. They enter the blood without the ability to return to the bone marrow. Neutrophil granulocytes have the ability to recognize foreign material, migrate across the vessel wall to the site of inflammation, absorb, kill and decompose or otherwise process phagocytosed contents. During bacterial inflammation, they make up the vast majority of all leukocytes (leukocytosis). Activated neutrophils in tissues produce chemotactic factors for monocytes and lymphocytes, thereby ensuring that these cells enter the site of inflammation, where they elicit a specific immune response.
A shift to the left which is an excessive number of immature forms of neutrophils in the peripheral blood usually accompanies neutrophilic leukocytosis. Severe bacterial infection is also accompanied by morphological changes in neutrophils – the presence of toxic granulations, Döhle's bodies and vacuolization. For example salmonellosis and brucellosis are characterized by high leukocytosis and a shift to the left (up to 60%), which are of almost diagnostic importance. On the other hand, neutrophilia is not common in viral infections. Systemic infections caused by fungi, protozoa, rickettsiae or spirochetes may be associated with neutrophilia.
In the initial phase of inflammation, there may be transient neutropenia due to the transfer of peripheral neutrophils to the marginal part. On the first day of inflammation, mostly more mature forms of granulocytes (rods and metamyelocytes) are released, and during the septic process, sometimes also myelocytes and myeloblasts.
In prolonged infection, neutropenia occurs due to the depletion of most of the bone marrow neutrophil storage. (This phenomenon can be mistaken for a remission of inflammation, so be careful when it is accompanied by a significant shift to the left!) [1]
Clinical signs of neutropenia[edit | edit source]
- mucosal infections (aphthous ulcers, periodontal disorders)
- skin infections (ulcers, abscesses, furuncles, prolonged wound healing)
- lymphadenopathy
- perineal and perirectal inflammation
- otitis media, bacterial and fungal pneumonia
- prolonged severe neutropenia → life-threatening infections of the gastrointestinal system and lungs
- most common infectious agents: Staphylococcus aureus, gram-negative bacteria (Pseudomonas aeruginosa)
- There is NO increased risk of parasitic and viral infections[1]
- CAVE! Patients with neutropenia lack a normal reaction to the infection - fever, pus production, pyuria in urinary tract infections, granulocytic pleocytosis in meningitis,…[2]
Causes of neutropenia[edit | edit source]
- congenital (rare; treatment with G-CSF or bone marrow transplantation), acquired (most common) and iatrogenic.
- Acquired
- infectious
- neutropenia in hypersplenism (reticuloendothelial sequestration)
- autoimmune (neonatal alloimmune neutropenia, systemic lupus erythematosus, Felty's syndrome)
- neutropenia is caused by bone marrow infiltration (leukaemia, neuroblastoma)
- Iatrogenic
- neutropenia in immunosuppressive therapy, cytotoxic therapy and radiotherapy
- drug-induced agranulocytosis (neutropenia): acetylsalicylic acid, indomethacin, ibuprofen; chlorpromazine, clozapine, diazepam, imipramine, risperidone; carbamazepine, phenytoin, valproic acid; carbimazole; amiodarone, captopril, digoxin, furosemide, hydralazine, thiazide diuretics, acyclovir, cephalosporins, clindamycin, gentamicin, lincomycin, macrolides, metronidazole, penicillins, glucocorticoids, mesalazine, sulfasalazine, omeprazole and others
- Congenital
- diseases affecting all lines:
- aplastic anaemia, amegakaryocyte thrombocytopenia,
- Shwachman-Diamond syndrome (blood examination: exocrine pancreatic insufficiency, low stature, metaphyseal dysplasia, medullary failure, risk of leukaemia),
- Fanconi anaemia (blood examination: dysplastic thumbs, pancytopenia, other anomalies),
- dyskeratosis congenita (changes in nails, skin and teeth)
- erythrocyte development disorders:
- Diamondo-Blackfan anaemia (erythropoiesis disorder, craniofacial and thumb anomalies)
- neutrophil development disorders:
- severe congenital neutropenia (Kostmann's syndrome) – AR hereditary severe neutropenia (< 0,5×109/l), inhibited maturation of precursors of granulopoiesis in the bone marrow at the level of promyelocyte-myelocyte, recurrent severe bacterial infections, in the first days of life skin infections, umbilical cord infections and stomatitis (St. aureus, E. coli, Pseudomonas aeruginosa), treatment with recombinant granulopoiesis growth factors (G-CSF) or a bone marrow transplantation;
- cyclic neutropenia – (AD hereditary or sporadic) cyclically recurring disorder of stem cell division in the bone marrow, manifestation at the age of around 10 years, at intervals of approximately 20 days neutropenia occurs with fever and ulcerations of the oral mucosa, abscesses, osteomyelitis and sepsis, treatment with antibiotic infections, good prognosis;[3]
- glycogenosis Ib – glycogen storage in the liver, fasting intolerance, hypoglycemic episodes, elevated lactate levels, colitis, neutropenia,
- Barth's syndrome – X-linked syndrome, dilated cardiomyopathy with endomyocardial fibrosis, myopathy and neutropenia,[4]
- vesicular transport disorders:
- Chédiak-Higashi syndrome (lysosomal trafficking regulator defect; albinism, NK and T-cell dysfunction),
- Griscelli syndrome type II, Heřmanský-Pudlák syndrome type II
- megakaryocyte development disorders:
- Wiskott-Aldrich syndrome (lymphocyte development and monocyte maturation disorder, eczema, immunodeficiency and thrombocytopenia),
- reticular dysgenesis (AR hereditary SCID – Severe Combined Immunodeficiency Disease), cartilage-hair hypoplasia, neutropenia with agammaglobulinemia or dysgammaglobulinemia[1]
Examination[edit | edit source]
- clinical picture, anamnesis (At what age did the child have the first infection? How often do the infections occur? How serious are they? Does the child have a growth disorder? What does the stool look like? Positive family history? Drug treatment?)
- blood examination + differential blood count
- reticulocytes
- Coombs test
- ANA, anti-dsDNA – systemic lupus erythematosus
- antineutrophilic antibodies
- IgG, IgA, IgM
- lymphocyte subtypes
- bone marrow examination
- DNA analysis (specific mutations)
- decreased serum trypsinogen, increased fecal fat content – Shwachman-Diamond syndrome[1]
Related articles[edit | edit source]
References[edit | edit source]
- ↑ a b c d e f MIHÁL, Vladimír. Neutropenie u dětí. Pediatrie pro praxi [online]. 2010, y. 11, p. 87-91, Available from <https://www.pediatriepropraxi.cz/>. ISSN 1213-0494.
- ↑ MUNTAU, Ania Carolina. Pediatrie. 4. edition. Praha : Grada, 2009. 251 pp. ISBN 978-80-247-2525-3.
- ↑ MUNTAU, Ania Carolina. Pediatrie. 4. edition. Praha : Grada, 2009. pp. 251-252. ISBN 978-80-247-2525-3.
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3127744/