Malignant arrhythmia
Rhythm disorders can be divided into tachycardia and bradycardia. Both may be caused by disturbances in the generation of excitation or its conduction.
- A 12-lead ECG recording is usually sufficient. It is insufficient, especially in conditions where the localization of the P wave is unclear or hidden in the QRS complex.
- We use the esophageal ECG mainly in the diagnosis of AV nodal reentry tachycardia, in differential diagnosis to differentiate atypical supraventricular tachycardias from ventricular tachycardias. In addition, esophageal electrodes can be used for atrial pacing, to stop/start reentry SVT.
Extrasystoles[edit | edit source]
Supraventricular extrasystoles (ES) are more common at younger ages, and ventricular ES is more common at later ages.
In terms of etiology, the following apply:
- hypoglycaemia,
- Internal environmental disorders,
- Endocrinopathies,
- Myocarditis,
- Cardiomyopathy.
ES can also occur in healthy hearts.
- Monotopic ones come from one and polytopic ones come from multiple locations - these have multiple P-wave (supraventricular ES) or QRS complexes (ventricular ES),
- If a normal sinus pulse alternates with an ES on the ECG, we speak of bigeminy,
- If the ES repeats after two sinus pulses, it is trigeminy,
- If one sinusoidal pulse is followed by a pair of ES, we use the term couplet,
- When they come in threes, we speak of a triplet - when there are three or more ECs, we speak of tachycardia,
- Ventricular ES: on ECG we find an aberrant QRS complex, preceded by a missing P wave, the T wave is usually discordant (i.e. oriented opposite to the highest oscillation of the QRS complex).
If the EC is found at rest but disappears on stress, this is a valuable indication of benignity.
- Potentially severe are
- ES multifocal,
- ES multiple,
- ES arising from the L ventricle,
- ES appearing on exertion and disappearing at rest,
- ES with R to T phenomenon, i.e. ventricular ES superimposed on the descending arm of the T wave - can lead to ventricular fibrillation.
Bradycardia[edit | edit source]
Bradycardia often accompanies hypoxic states, in which case causal management is required, i.e. adequate oxygen therapy.
Sinus node dysfunction - sick sinus syndrome[edit | edit source]
This is a disorder of impulse generation. It can be functional or anatomical and transient or permanent.
Etiology[edit | edit source]
- Increased vagotonia,
- Endocrinopathy,
- Pharmaceuticals,
- Direct damage to the sinus node.
Clinical manifestations[edit | edit source]
Most patients are asymptomatic; young children may have feeding problems, larger children may have fatigue, vertigo. However, some children are at risk of syncope or sudden death.
Diagnostics[edit | edit source]
- On ECG we can observe slow or irregular sinus action, various alternate rhythms or, on the contrary, paroxysms of tachycardia,
- Negative influence of the autonomic nervous system is confirmed by the ability of the sinus node to increase HR during exercise (confirmed by ergometry),
- Holter ECG shows the variability of HR during day and night, episodes of sinus pauses or the occurrence of other severe rhythm disturbances.
Therapy[edit | edit source]
- Asymptomatic patients do not require therapy,
- In bradycardia with impaired hemodynamics, we indicate implantation of a cardiac pacemaker.
Second-degree atrioventricular block, Mobitz type II[edit | edit source]
It is characterized by intermittent atrioventricular (AV) conduction blockade without preceding PQ prolongation, i.e. the PQ interval is still constant, after several "normal" contractions the P wave is not monitored by the QRS complex.
Etiology[edit | edit source]
- Direct injury by trauma,
- Inflammation,
- Degenerative disease.
![]() Mobitz II requires very careful monitoring because, unlike Mobitz I, there is a real threat of progression to grade III block, i.e. complete AV block with risk of syncope or sudden death.
Mobitz II requires very careful monitoring because, unlike Mobitz I, there is a real threat of progression to grade III block, i.e. complete AV block with risk of syncope or sudden death.
Therapy[edit | edit source]
- Isoprenaline 0.02 mg/kg, eventually isoprenaline infusion 0.02 mg/kg (interestingly, Atropine has no effect here),
- The long-term solution is the implantation of a pacemaker.
Third-degree atrioventricular block - complete AV block[edit | edit source]
- Complete interruption of impulse transmission from the atria to the ventricles,
- the atria are driven by rhythm from the sinus conduction system, the ventricles by an alternate slower rhythm from the junction or ventricles.
Etiology[edit | edit source]
- Surgical damage,
- Inflammation,
- Cardiomyopathy,
- Newborns of mothers with SLE.
Clinical manifestations[edit | edit source]
Clinically manifested by a picture of low cardiac output.
Diagnostics[edit | edit source]
The ECG shows independent atrial and ventricular activity. The P wave frequency is higher than the QRS frequency, there is no constant time interval between P and QRS, the QRS has an abnormal shape but is usually narrow.
Therapy[edit | edit source]
- Atropine: 0.02 mg/kg i.v., i.o., e.t., i.e., 0.1 mg/5 kg (0.2 ml),
- Alternatively, Isoprenaline 0.02 mg/kg,
- Cardiac pacing as a definitive solution.
In a child who has signs of heart failure and a systolic rate below 60/min, a grade III AV block must be ruled out by ECG.
Tachycardia[edit | edit source]
Pathophysiology[edit | edit source]
Tachycardias arise from 3 possible mechanisms:
- The principle of abnormal automaticity - tachycardias are initiated by spontaneous depolarization of a cell that is not part of the sinus node, these tachycardias are therapeutically very difficult to influence, as neither cardioversion nor overdriving works in them, digoxin and beta-blockers are used in treatment,
- The principle of triggered activity - tachycardia is caused by afterdepolarizations,
- Principle of the reentry circuit - is the mechanism of most arrhythmias, reentry is a phenomenon of the intact heart and involves a circular conduction of excitation between two different cardiac pathways, where the pathways must be functionally separated.
It should be kept in mind that even in sinus rhythm there are limits to the tolerance of tachycardia. One recommendation is based on the equation for determining the maximum tolerable frequency to the age of the patient:
HRmax = 220 - age in years
A heart rate exceeding this value can already reduce cardiac output by the principle of reduced diastolic filling. Patients with low ventricular compliance are the most compromised. Tachyarrhythmias are divided into:
- Supraventricular (SVT) - occur above the bifurcation of the Bundle of Hiss,
- Ventricular (VT) - beneath the bifurcation of the bundle of His.
If the QRS complex is " narrow", i.e. < 0.08 seconds, we assume that one of the supraventricular mechanisms is the cause of the tachycardia. If the QRS is "wide", i.e. > 0.10 seconds, it may be a ventricular tachyarrhythmia or atypical SVT. In practice, it is quite difficult to differentiate VT from atypical SVT on the basis of standard ECG alone (an excellent diagnostic method here is the oesophageal ECG) - tachycardia with a "wide" QRS in the acute situation is always treated as VT until proven otherwise.
Tachyarrhythmias with a "narrow" QRS = SVT[edit | edit source]
SVT is rarely life-threatening unless it lasts too long, so the first rule of SVT treatment is calm and deliberation with simultaneous efforts to determine the mechanism of the cause of the tachycardia before starting treatment. On the other hand, prolonged SVTs or some SVTs in WPW require urgent therapeutic intervention.
Diagnostics[edit | edit source]
To determine the exact mechanism of the arrhythmia (i.e., temporal relationship of the P wave and QRS complex, determination of the P wave axis), a 12-lead recording is much more useful than a single-lead recording. Paroxysmal SVTs with narrow QRS and reentry mechanism have RP interval shorter than PR. The diagnosis is based on:
- Medical history,
- Physical examination,
- 12-lead ECG,
- Echocardiography,
- Ergometry,
- Holter ECG,
- Transtelephonic ECG transmission,
- Atrial pacing,
- Intracardiac electrophysiological studies.
Therapy[edit | edit source]
Acute Therapy:
- Vagal maneuvers - the diving reflex most commonly used today - applying ice to the face,
- Adenosine (Adenocor) 0.1 mg/kg i.v., i.o. very quickly,
- Preferably followed by a bolus of FR as adenosine has an extremely short half-life,
- At a repeated dose of 0.2 mg/kg i.v.
Further according to experience:
- Propafenone (Rytmonorm) 1-2 mg/kg i.v. within 5 minutes,
- Esophageal atrial pacing,
- Eventually, electrical cardioversion.
Follow-up therapy:
- Beta blockers,
- Digoxin (cave! - KI in WPW syndrome),
- Propafenone,
- Amiodarone,
- Sotalol,
- In older children with SVT reentry, we prefer radiofrequency catheter ablation
Sinus tachycardia should be differentially diagnosed. Here, unlike SVT, HR is usually < 200/min, speeds up and slows down according to sympathetic tone (reentry tachycardia arises and subsides abruptly, has no frequency variation), the P-wave axis is always normal, the A:V conversion ratio is typically 1:1. Therapeutically, the underlying disease must always be treated! The most common causes of sinus tachycardia are:
- Fever,
- Anemia,
- Shock,
- Heart failure,
- Pain/stress,
- Hyperthyroidism.
Tachyarrhythmias with "wide" QRS = Atypical SVT and VT[edit | edit source]
VT consists of three or more aberrant QRS complexes that are wider than during sinus rhythm. Diagnosis is based on history, physical examination - here the key question is whether the patient requires CPR, 12-lead ECG. Ventricular tachyarrhythmias are the most malignant rhythm disturbances, typically occurring in patients with impaired myocardial function.
- Most forms of VT also arise by a reentry mechanism,
- QRS complexes are wide and either have identical morphology = monomorphic or have different QRS shapes = polymorphic - more malignant forms,
- In many cases the P wave is not visible at all.
Therapy[edit | edit source]
Acute therapy:
- If the patient is hypotensive or unresponsive, we perform urgent electrical cardioversion,
- If cardioversion is not available, administer Amiodarone (Cordaron) 5 mg/kg i.v. within 30 minutes as first choice drug, possibly repeated in 15-20 minutes,
- Alternatively, 1% Mesocaine or Lidocaine 1 mg/kg i.v. can be given as a bolus followed by 20-60 ug/kg/min in a continuous infusion,
- In ventricular fibrillation, perform unsynchronized cardioversion.
Specific therapeutic alternative with knowledge of QRS morphology:
- Monomorphic reentry VT: procainamide 10-15 mg/kg i.v. over 20 minutes,
- Torsade de pointes: MgSO4 25-50 mg/kg i.v. over 15-30 minutes, max 2 g for dosing, treat ionic imbalances by supplementation of missing ions,
- Any VT: electrical cardioversion, initial discharge 1-2 J/kg, can be repeated 1-2 times with discharge up to 4 J/kg
Follow-up therapy:
- For the permanent safety of congenital forms with prolonged QT, beta-blockers are useful.
Torsade de pointes[edit | edit source]
A specific form of VT is the form known as torsade de pointes. This is a polymorphic VT in which the direction of the QRS complexes gradually rotates around the isoelectric line of the ECG. Torsades classically occur in patients with an abnormally prolonged QT interval - when associated with deafness we speak of the Jervell-Lang-Nielsen syndrome, if hearing is normal we speak of Roman-Ward syndrome, another etiological group are patients with ion imbalances such as hypokalemia, hypocalcemia and hypomagnesemia. Clinically, torsades can cause hypotension, syncope, and eventually ventricular fibrillation and death.
Atrial fibrillation and flutter[edit | edit source]
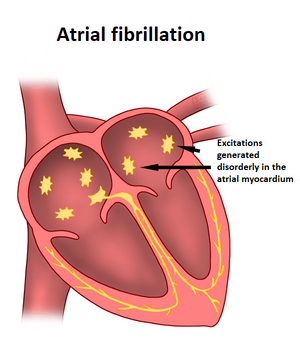
- Atrial fibrillation and flutter are caused by a reentry mechanism in the atrial muscle,
- Flutter represents a single reentry circuit, whereas fibrillation is multiple small and constantly changing reentry circuits,
- Atrial fibrillation and flutter are also the most severe form of arrhythmia in WPW syndrome with the possibility of rapid antegrade transmission to the ventricles - a catastrophically rapid ventricular response with the risk of cardiac arrest!
Etiology[edit | edit source]
- Atrial dilatation,
- Inflammation,
- Hyperthyroidism,
- WPW syndrome.
Diagnosis[edit | edit source]
- Atrial flutter classically looks like sawtooth = F waves on ECG,
- They are best seen in leads II, III and aVF and have a very irregular frequency of about 300/min (there may be an isoelectric line between each F wave),
- Atrial fibrillation has the appearance of irregular, low-voltage, fast atrial waves = f waves on the ECG,
- The ventricular frequency in both conditions is determined by the ability of the conduction system to convert excitations to ventricular - risk of ventricular tachyarrhythmias.
Therapy[edit | edit source]
- Due to the mechanism of both arrhythmias is reentry, synchronized cardioversion is elegant and virtually always successful,
- Alternatively, Digoxin can be administered pharmacologically (to increase the degree of AV block - reducing the transmission to the ventricles),
- overdriving can be attempted in flutter (ineffective in fibrillation for multiple rapid reentry circuits).
Key terms[edit | edit source]
Synchronized cardioversion[edit | edit source]
This is a discharge designed to terminate SVT or organized VT, therefore must be synchronized with the QRS complex. Coincidence with a T wave could induce ventricular fibrillation.
Defibrillation[edit | edit source]
This is a discharge using more energy, which is indicated in polymorphic VT or in ventricular fibrillation - here there is no QRS with which the discharge can be synchronized.
Overdrive pacing = overdriving[edit | edit source]
This involves stimulating a portion of the affected myocardium at a frequency slightly higher than the conduction capability of the reentry circuit.
Sources[edit | edit source]
External links[edit | edit source]
- Ventricular tachycardia and ECG - Free ECG book
Related articles[edit | edit source]
Source[edit | edit source]
- MUDr.HAVRÁNEK, Jiří: Maligní arytmie