Cardiac conduction system
Function[edit | edit source]
Cardiac muscle cells ( cardiomyocytes ) can be divided into 2 groups based on their function:
- Cells - having the ability to autonomously generate impulses and subsequently distribute these impulses throughout the heart. Such cells are collectively referred to as the cardiac conduction system (PSS).
- Cells - whose primary function is contraction . They have the ability to generate excitement only under pathological conditions. Such cells are collectively referred to as working myocardium .
Summary:
- PSS cells generate and relatively rapidly distribute impulses in a certain sequence throughout the myocardium (thereby signaling the working myocardial cells to contract).
- The cells of the working myocardium perform their own contraction (contraction) of the heart muscle
Properties[edit | edit source]
PSS has 3 basic properties. They are:
- Autonomy (independence). Within the organism, the heart has a certain degree of independence. Individual heart contractions occur in the heart itself (in the PSS) independently of the CNS and humoral mechanisms. The autonomic nervous system (sympathetic and parasympathetic) can only regulate the frequency of heart contractions, not the contractions themselves. Generally:
- the sympathetic nerve increases the heart rate via the nervi cardiaci ( noradrenaline , α-adrenergic receptors);
- the parasympathetic via the rami cardiaci nervi vagi ( acetylcholine , muscarinic receptors) reduces the heart rate.
- Automation (self-activity). The heart is capable of automatically generating regularly repeating stimuli for its own contraction .
- Rhythmicity (regularity). Stimuli for contraction (excitement) are generated by the heart regularly, i.e. with a certain frequency.
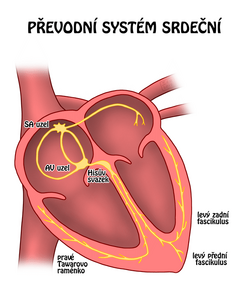
Structure[edit | edit source]
- SA node (sinoatrial node, nodus sinoatrialis )
- Internodal atrial connections
- AV node (atrioventricular node, nodus atrioventricularis )
- His bond
- Tawar arms (left and right)
- Purkinje fibers
SA node[edit | edit source]
The SA node is located below the epicardium in the wall of the right atrium near the mouth of the venae cavae superioris . It is the so-called primary pacemaker (rhythm setter) - under physiological conditions, the excitation is generated in the SA node. This is due to the fact that spontaneous diastolic depolarization occurs faster in the SA node than, for example, in the AV node or in specialized ventricular cardiomyocytes.
Internodal atrial junctions[edit | edit source]
From the SA node, the excitation (wave of depolarization) spreads to the working myocardium atria. The impulse reaches the AV node via the so-called preferential pathways , which are:
- Bachman's pathway – interatrial bundle going from the right to the left atrium;
- Wenckebach volume ;
- James's volume ;
- The Volume of Thorel .
Preferential pathways conduct excitation faster than "normal" working myocardium atria.
AV node[edit | edit source]
The AV node is located under the endocardium in the wall of the right atrium near the mouth of the coronary sinus above the septal leaflet of the tricuspid valve. The AV node conducts the impulse very slowly, which results in a desirable delay in the atrioventricular conduction (AV conduction, atrioventricular conduction) - first the contraction (depolarization) of the atria needs to be completed, and only then the contraction (depolarization) of the ventricles begins. In case of damage to the SA node, the AV node takes over the role of the pacemaker – it is also referred to as the secondary pacemaker . Since spontaneous diastolic depolarization is slower here, the heart rate originating in the AV node is also slower than the frequency originating in the SA node.
The rhythm originating from the SA node is referred to as sinus , from the AV node as nodal .
His Volume[edit | edit source]
The fibrous skeleton between the myocardium of the atria and the myocardium of the ventricles acts as a barrier that prevents the impulse from the atria to the ventricles. The impulse from the atria can reach the ventricles only through the bundle of His, which connects to the AV node. The bundle of His penetrates through the fibrous skeleton (through the trigonum fibrosum dextrum ) into the interventricular septum. The AV node and the upper part of the bundle of His are referred to as the AV junction (atrioventricular junction, the connection between the atria and ventricles).
Tawar's shoulder blades[edit | edit source]
At the interventricular septum, the bundle of His divides into two branches: the right and left branches of Tawar . The right bundle of Tawar will conduct the impulse to the right ventricular myocardium. The left bundle of Tawar further branches into the anterior bundle (fasciculus anterior) and the posterior bundle (fasciculus posterior). The left bundle of Tawar conducts the impulse to the interventricular septum and the myocardium of the left ventricle.
Purkinje fibers[edit | edit source]
Tawar's branches subsequently branch into Purkinje fibers , which distribute the impulse to the working myocardium of the ventricles.
Summary:
SA node → internodal atrial junctions → AV node → bundle of His → bundles of Tawar → Purkinje fibers.
Vascular supply of nodes of the transmission system
- In 60% of cases, the SA node is supplied by the branches of a. coronariae dextrae ( a. nodi sinuatrialis , a. principalis atrialis dextrae ).
- In 90% of cases, the AV node is supplied by the branches of a. coronariae dextrae ( a. nodi atrioventricularis , r. septi fibrosi , Haas's artery).
Spontaneous diastolic depolarization[edit | edit source]
A resting membrane potential does not occur in sinoatrial and atrioventricular node cells . Instead, each action potential is preceded by a gradual change in the membrane potential towards the threshold value. This event is called spontaneous diastolic depolarization and depends on the autonomic nervous system.
The essence of the action is the movements of the following ions:
- Na + intracellularly
- Ca 2+ intracellularly
- decreased K + current extracellularly
Na+ ions enter the cell through funny channels and are less important in terms of overall depolarization. Ca2+ ions have the largest share in the occurrence of spontaneous diastolic depolarization. There is an influx of Ca2+ into the cell through specific channels. The influx of calcium ions causes gradual depolarization and the subsequent formation of an action potential. The last of the events mentioned is the reduction of the flow of K+ out of the cell. This gradual inactivation plays a crucial role in the occurrence of spontaneous diastolic depolarization − under normal circumstances, the K+ current is responsible for maintaining the resting membrane potential.
Links[edit | edit source]
Related resources[edit | edit source]
External links[edit | edit source]
- Electrical Conduction System of the Heart - Free ECG book
sources[edit | edit source]
- PASTOR, Jan. Langenbeck's medical web page [online]. [cit. 2009]. <https://langenbeck.webs.com/>.
References[edit | edit source]
- TROJAN, Stanislav. Lékařská fyziologie. 4. edition. Praha : Grada, 2004. 772 pp. ISBN 80-247-0512-5.
- HAMAN, Petr. Výukový web EKG [online]. [cit. 29.4. 2010]. <http://ekg.kvalitne.cz/system.htm>.