Interventional Radiology
Interventional radiology is a method that allows us to replace or facilitate surgery under the supervision of imaging technology. Since these are more or less invasive interventions, we must always consider whether the risk is greater than the benefit for the patient. These interventional radiological methods can be divided into vascular and non- vascular.
Vascular intervention[edit | edit source]
These are mini-invasive medical procedures that we perform directly on or through the vascular system They are based on catheter angiography. The most common include: percutaneus transluminal angioplasty, use of stents a stentgrafts, local trombolysis, transcatheter embolization, insertion of filters into the inferior vena cava and TIPS.
Local thrombolysis[edit | edit source]
Local thrombolysis is a process where we introduce a catheter directly into the obliteration site, and thus the use of thrombolytic agents is more selective and has fewer systemic effects. Indications for local thrombolysis are fresh thrombi - cerebral infarction, e.g. within 3 hours of the onset of symptoms.
- Local continuous thrombolysis - we insert the catheter into the proximal part of the thrombus and continuously administer the thrombolytic agent with an infusion pump.
- Local accelerated thrombolysis - this method combines mechanical thrombus breaking with the use of thrombolytics.
Complications can be bleeding, peripheral embolization of thrombus remnants, allergic reaction to the thrombolytic agent, and complications associated with catheter insertion.
Transcatheter embolization[edit | edit source]
We use transcatheter embolizations in some cases of uncontrollable bleeding, to reduce vascularization in tumors and thereby slow down their growth, to remove AV malformations, aneurysms and hemobilia. Examples:
- closure of small arteries in AV malformations in the brain with glue (followed by surgical resection / gamma knife irradiation);
- closure of nutrient vessels, e.g. in large meningiomas before neurosurgery ;
- closure of cerebral bulges with spirals (coiling aneurysms); in elderly patients with a high risk of surgery, in aneurysms in the vertebrobasilar bed;
- the advantage is access with just an injection in the groin, a smaller number of complications that would be associated with the operation and a shorter hospitalization period;
- the disadvantage (so far) is the lower reliability of aneurysm closure from a long-term perspective compared to a surgical clip;
- currently, an intracranial stent can be used for greater stability of the coil, and the coils themselves are coated with an absorbable matrix, so that the aneurysm is gradually shrunk.
Inferior vena cava filters[edit | edit source]
The insertion of a filter into the inferior vena cava is indicated for patients for whom anticoagulant treatment is not suitable and who suffer from thromboembolic disease.
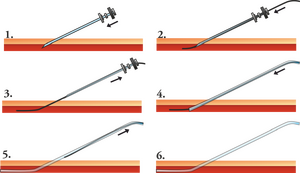
Kavafilters are inserted using the Seldinger technique through the femoral or jugular vein. It is important that they are inserted in the right place - with few exceptions always below the mouth of the renal veins, therefore we must perform a cavography before the procedure, preferably in two projections.
- Complications include misplacement of the filter, inferior vena cava perforation, inferior vena cava thrombosis, migration when the wrong dimensions are selected or insufficient fixation, and complications associated with catheterization.
Nonvascular Interventions[edit | edit source]
Non-vascular procedures are performed outside the vascular system. We include interventions on the biliary tract, GIT, respiratory tract and percutaneous drainage of abscesses.
Biliary tract interventions[edit | edit source]
The most common procedures include:
- percutaneous transhepatic drainage of the bile ducts :
- indications are obstruction of the bile ducts accompanied by sepsis or liver decompensation, preoperative decompression of the bile ducts and above all treatment of otherwise intractable diseases of the bile ducts and palliative treatment of malignant stenoses;
- there are no absolute contraindications;
- before the procedure itself, we perform an US, ERCP or CT examination;
- dilatation of stenoses of bile ducts;
- percutaneous extraction of stones from the bile ducts.
Intervention on GIT[edit | edit source]
In this system, we mainly intervene when:
- dilation of stenoses of the upper part of the GIT using a balloon catheter or stents. The causes can be benign - cauterization of the esophagus - but more often it is malignancy of the esophagus and cardia;
- percutaneous gastrostomy - especially in patients who cannot take food in any other way for a long time.
Links[edit | edit source]
Related Articles[edit | edit source]
Related images[edit | edit source]
- Dialysis Shunt Angioplasty (atlas.mudr.org)
- Stenotic Renal Artery Stenting (atlas.mudr.org)
- Embolization, RFA of a kidney tumor (atlas.mudr.org)
References[edit | edit source]
- SAMEŠ, M. Neurochirurgie. 1. edition. Jessenius Maxdorf, 2005. ISBN 80-7345-072-0.
- JOSEF NEKULA, Miroslav Heřman. Radiologie. První edition. Univerzita Palackého v Olomouci, 2001. 205 pp. ISBN 80-244-0259-9.