Eating disorders.
Protein and energy malnutrition[edit | edit source]
Insufficient intake of protein and energy in the diet leads to a loss of total body mass and adipose tissue, although not evenly. Protein and energy malnutrition primarily arise when the quality and quantity of nutrition is deficient in the long term. In some developing countries, it occurs endemically, with a prevalence of up to 25%. This is especially a problem where the main component of food is plant proteins with low biological value at the current high incidence of infectious diseases. In case of insufficient energy supply, proteins are oxidized as an energy source and are not used for the synthesis of body proteins. The main manifestations of children in developing countries are two syndromes: kwashiorkor and marasmus.
Kwashiorkor[edit | edit source]
It is thought to be caused by a selective protein deficiency. It is manifested by short stature, edema, hypoalbuminemia, liver steatose, preservation (preservation) of subcutaneous fat.
Marasmus[edit | edit source]
A condition caused by a general lack of energy. It is manifested by the physical and mental reunion of the organism.
Secondary form of protein-energy malnutrition[edit | edit source]
It also occurs in industrialized countries as a result of pathological conditions leading to insufficient nutritional intake due to the needs of the organism. The main causes can be:
- Reduced oral intake::
- Increased nutrient losses :
- Increased need ::
Malnutrition can develop slowly (chronic partial starvation) or rapidly due to a severe acute illness. With uncomplicated starvation or partial starvation, the body can gradually adapt.
Eating disorders[edit | edit source]
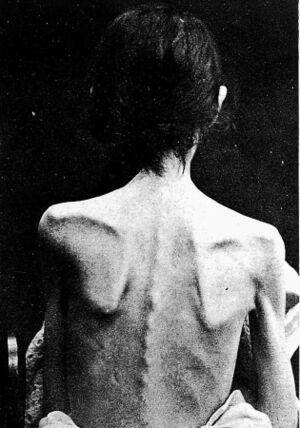
Anorexia nervosa[edit | edit source]
It is a chronic disease characterized in terms of behavior by inducing underweight by its own causes, from a psychological point of view the idea that thinness is an ideal of beauty, from a biological point of view a number of disorders (eg amenorrhoea) caused by insufficient food intake. Metabolic disorders include loss of subcutaneous fat, decreased core body temperature, decreased blood pressure and heart rate.
Skin discoloration (yellow discoloration) is caused either by hypercarotinemia from excessive supply of β-carotene in a one-sided diet or by a disorder of degradation and utilization of carotenoids. Women with amenorrhoea have both reduced FSH and LH, and periodic LH release during the day does not respond to a secretory stimulus via LH-RF (luliberin). The level of T 3 tends to decrease as its inactive reverse T 3 isomer (rT3) rises. In malnutrition and liver stress, they prefer deiodination of T 4 to rT 3 . T 4and TSH response to TRH are normal. Plasma cortisol levels are normal or slightly reduced, and urinary excretion of 17-hydroxycorticoids is reduced. The response to ACTH stimulation tends to be increased, to metyrapone normal. Growth hormone levels are normal or slightly elevated, while somatomedin levels are decreased.
The hematological findings are leukopenia,thrombocytopenie, anemie, but resistance to infection is good.
Bulimia nervosa[edit | edit source]
It is a behavioral disorder characterized by episodes of excessive overeating , accompanied by feelings of "cleansing" induced vomiting, diarrhea (laxativa) or increased diuresis (diuretics). Unlike anorexics, bulimics have a normal body weight . Neurotransmitters such as serotonin, dopamine norepinephrine, opioids and cholecystokinin are involved in the development and modulate feelings of hunger and satiety. Hypokalemic hypochloremic alkalósisis usually found for persistent vomiting.
Obezity[edit | edit source]
Obezity and overweight are caused by the accumulation of body fat. A simple measure is Quetelet's body mass index (BMI), which is calculated according to the formula below:
| BMI | Degree of obesity | |
|---|---|---|
| < 20 | Underweight | |
| 20–24,99 | Normal weight | |
| 25–29,99 | Overweight | I |
| 30–30,99 | Obesity | II |
| > 40 | Morbid obesity | III |
Adiposity alone is not such a risk, but the location of accumulated fat is important. Abdominal fat, especially abdominal fat (central obesity), is considered to be the most risky in terms of metabolic disorders. Abdominal adiposity can be measured indirectly using a measure index around the waist and around the hips (waist / hips). Visceral fat is an active metabolic tissue releasing fatty acids. Increased fatty acid intake to the liver and peripheral tissues induces insulin resistance and, together with alterations in the ratio of lipoprotein lipase and liver triacylglycerol lipase activity, is the cause of dyslipidemia in obesity.
The fat cell (adipocyte) forms a reservoir of body energy by expanding or contracting according to the state of energy balance. It arises from a precursor - a preadipocyte - to adapt to the continuing increased energy intake in the diet. Adipocytes gradually change their size during excessive intake up to a certain limit, which is 1 μg of weight. Then, preadipocyte differentiation is stimulated and new fat cells are produced, which can increase indefinitely, so that their total number in adipose tissue increases. However, once an adipocyte has formed, its dedifferentiation is very difficult. When energy intake is reduced, their number does not decrease, only their size decreases.
Genetic factors[edit | edit source]
To date, 23 genes have been identified that are associated with obesity. The mechanism of their action is not yet fully elucidated. It is estimated that more than 40% of cases of primary obesity are genetically determined. Recently, attention has been focused on the so-called OB gene, which is responsible for leptinsynthesis.
Leptin is a proteohormone of M r= 16,000 belonging to the family of hematopoietic cytokines, which is a product of the OB gene on chromosome 7q31.3 and which plays a key role in the regulation of body weight. It is produced by differentiated adipocytes. The main factor determining the level of circulating leptin is the amount of adipose tissue. Concentration increases with body mass index BMI or body fat fraction. Even small variations in body fat result in significant differences in leptin levels - from 0.03 μg / l in anorexic patients to values> 100 μg / l in extremely obese individuals. Leptin levels are age dependent (up to 20 years old). The biological effect of leptin is mediated by the leptin receptor (OB-R), which belongs to the class I family of cytokine receptors. Leptin causes a reduction in food intake (in experimental animals) and increased energy expenditure, including thermogenesis. In addition, leptin affects a number of endocrine systems. This effect is mediated by the action on hypothalamus,for the production of neuropeptide Y (NPY) - leptin suppresses the expression and secretion of NPY, which is a stimulator of food intake and regulates a number of pituitary hormones. In very simple terms, leptin is a signal from adipose tissue that informs the body of the energy stores stored in fat depots ..
Diet[edit | edit source]
The genetic factors underlying obesity alone are not enough. Lifestyle and environmental factors allow these talents to manifest themselves. The biggest role is played by the supply of energy-rich nutrients (hyperphagia = overeating) in proportion to physical activity.
Endocrine causes[edit | edit source]
Some endocrine disorders are associated with adipose tissue accumulation and obesity. These include hypothyroidism, acromegaly, Cushing's syndrome, hyperprolactinemia (this is usually attributed to postpartum obesity). Growth hormone deficiency and hypogonadism are associated with adiposity, but not necessarily with obesity. Type 2 diabetes mellitus, which is also often associated with obesity, is likely to have the same genetic predisposing factors. Increased insulin resistance and abdominal obesity are part of the so-called Reaven's metabolic syndrome (syndrome X).
Reaven's syndrome[edit | edit source]
It is an association of several risk factors, probably based on zřejmě insulin resistance associated with obezity, hypertension, hypertriacylglycerolemia, hyperglycemií, which were added by others such as hyperuricemia , hirsutism, disorders of blood clotting and fibrinolysis, microalbuminuria and the formation of so-called. Importantly, all of these signs are associated with the development of premature atherosclerosis. However, the metabolic syndrome and its causes cannot be understood as a manifestation of wear and tear or aging, but it is based on genetically modified terrain.
Insulin resistance is the result of an alteration in the release of insulinfrom β-cells rather than a change in the threshold for glucose stimulation. An enlarged fat cell is less sensitive to the antilipolytic and lipogenic effects of insulin. Although a reduced number of insulin receptorsis also involved in the development of insulin resistance, its result is much greater than the decrease in the number of receptors. Thus, there must be a postreceptor defect. It also occurs in other insulin-sensitive tissues, especially in muscle. As insulin resistance deepensglucose uptake by peripheral tissues decreases and hepatic glucose output increases.
Links[edit | edit source]
[edit | edit source]
Other chapters from the book MASOPUST, J., PRŮŠA, R .: Pathobiochemistry of metabolic pathways
Source[edit | edit source]
- MASOPUST, Jaroslav and Richard PRŮŠA. Pathobiochemistry of metabolic pathways. 2nd edition. Charles University, 2004. 208 p.