Bladder Cancer
From WikiLectures
They currently make up more than 2% of newly diagnosed malignancies.
Epidemiology[edit | edit source]
- Morbidity is still rising, mortality is decreasing, it affects men 3 times more often ,
- high incidence - in SW Europe, low in India and Japan,
- the main occurrence is between the 50s and 70s.
Etiology[edit | edit source]
- The main risk factor is smoking (mainly black tobacco smoking),
- exposure to certain industrial pollutants - aromatic amines (benzidine, 2-naphthylamine,…),
- chronic infection, in endemic areas - schistosomiasis (does mainly squamous cell ca).
Clinical manifestations[edit | edit source]
- Hematuria and pollakiuria ,
- increased bladder irritation indicates involvement of the throat, hydronephrosis and secondary pyelonephritis may occur in the area of the urethral orifice ,
- sometimes it can be completely asymptomatic,
- general symptoms (anorexia, weight loss, anemia ) - are only in very advanced tumors.
Diagnostics[edit | edit source]
- Cystoscopy ,
- endoscopic biopsy , or transurethral resection → it is necessary to determine the level.
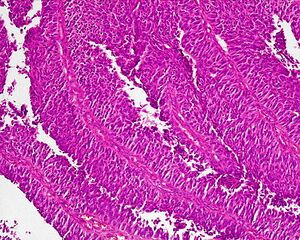
Histopathology[edit | edit source]
- 97% are carcinomas from the urothelium , rarely adenocarcinomas and undifferentiated carcinomas , squamous cell carcinomas are endemic (schistosomiasis),
- macro - different appearance - papillary, infiltrating, probably in ¼ they arise multicentricly (this is the cause of frequent recurrences),
- they can start as ca in situ and then change into a papillary or infiltrating form,
- initially the tumor grows in the mucosa, then grows early into the submucosa, muscle and surrounding fat, metastasizes to the pelvic nodes , later paraaortic , more rarely hematogenously.
Therapy[edit | edit source]
The method of therapy depends on a careful evaluation of histology, degree of invasion, extent of the disease.
Surgical treatment[edit | edit source]
- Non-invasive tumors can be treated by transurethral resection (TUR) - it is a relatively minor damaging procedure, it does not affect bladder function,
- for the treatment of surface structures - coagulation or laser vaporization ,
- but often there is a recurrence within 1 year, so the five-year survival does not exceed 80%,
- therefore, it is recommended to supplement adjuvant intravesical CHT, intravesical application of IFN, BCG vaccine, adriamycin, irradiation,
- if the tumor grows into the muscle - partial cystectomy ,
- the rationality of this procedure is questioned given the multifocal origin of urothelial
- moreover, there is a risk of implantation targets, so it is practically not implemented today,
- for larger tumors - radical cystectomy with lymphadenectomy , in men with prostatectomy in women with hysterectomy , adnexectomy ,
- it is a very demanding performance and its indications must be carefully considered.
Radiotherapy[edit | edit source]
- It is most often not used as an external radiation, as a separate treatment, for numerous emergency services,
- even as a neoadjuvant , no significant effect has been confirmed,
- So far, radiochemotherapy (RCHT) could have a good effect, but this is not substantiated by studies
- however, it is irreplaceable as palliation (skeletal meta analgesia, suppression of hemorrhagic complications).
Chemotherapy[edit | edit source]
- It is administered either locally or systemically ,
- local - in diffuse ca in situ, in superficial tumors after TUR and in papillary (the most advantageous today seems mitomycin C , which is practically not absorbed from the bladder and does not endanger toxicity),
- systemic - the main palliative treatment of advanced forms, the tumor responds to a number of cytostatics,
- corresponds most to - Pt derivatives, anthracyclines, ifosfamide ,
- adjuvant CHT - very useful especially for nodal involvement,
- neoadjuvance - has many disadvantages, it is not done by default.
Photodynamic therapy[edit | edit source]
- It can act in ca in situ and in papillary ca.
Immunotherapy[edit | edit source]
- Mainly in the form of local application of BCG .
Prognosis[edit | edit source]
- In non-invasives, 5-year survival is 75-80%.
Links[edit | edit source]
[edit | edit source]
External links[edit | edit source]
Source[edit | edit source]
- BENEŠ, Jiří. Study materials [online]. © 2010. [feeling. 16-06-2010]. < http://jirben.wz.cz >.