Anemia from decreased erythrocyte production
| Risks factors | malabsorption in celiac disease, Crohn's disease; chronic bleeding |
|---|---|
| Clinical picture | difficulty swallowing, nail changes, fatigue, neurological symptoms (eg. paresthesia) |
| Diagnosis | decreased plasma iron levels, low serum ferritin, increased plasma transferrin, presence of siderocytes, anisocytosis, poikilocytosis |
| Therapy | iron supply |
| Clasification and links | |
Iron deficiency anemia - sideropenic anemia (microcytic, hypochromic)[edit | edit source]
Sideropenic anemia is caused by a deficiency in hemoglobin synthesis due to iron deficiency. This is the most common anemia in childhood. [1]
Causes[edit | edit source]
Insufficient iron intake in the diet is rare in our country. Substances that inhibit resorption (phosphates, phytates) can cause a reduced supply. It is more common during malabsorption (celiac disease, Crohn's disease, after resection of the stomach or intestines). It also arises from excessive blood loss during chronic bleeding (peptic ulcers, hemorrhoids, cancer of the GIT, menorrhagia, metrorrhagia). Iron deficiency also manifests itself if the body has increased demands on hematopoiesis (during pregnancy, childhood).
Hemoglobin structure - α and β subunits are red and blue, iron-containing heme is green
Causes of sideropenic anemia in children
- Absorption disorder - treatment with antacids, drugs that increase gastric pH, drinking tea and coffee;
- Insufficient / unavailable iron stores - bleeding, epistaxis, gastric and duodenal ulcers, Meckel's diverticulum, allergies to cow's milk protein, parasites, Helicobacter pylori infections, esophageal varices, tumors and polyps of the gastrointestinal tract, inflammatory diseases of the GIT, AV maliculitis, heavy menstrual bleeding, uropoietic tract infections / tumors, pulmonary haemosiderosis;
- Congenital / acquired disorders of iron metabolism - atransferinemia, disorders of heme synthesis. [1]
Iron in the human body[edit | edit source]
There are a total of 3-4 g of iron in the body, most of which is found in hemoglobin. By recycling iron from the decaying erythrocytes, 20 mg per day is obtained, in the adult < 5 % of iron comes from the diet, in the infant 30 %.
The full-term newborn has sufficient iron reserves for the first 6 months, after which a supply of iron is necessary. Premature babies have lower hemoglobin concentrations and lower iron stores, so iron depletion occurs as early as the 2nd month. Breast and cow's milk have the same iron content, but it is less well absorbed from cow's milk. The iron content of breast milk decreases after 5 months of breastfeeding. Boys need a higher iron intake during puberty due to an increase in muscle mass and myoglobin. Girls need a higher iron intake due to menstrual bleeding losses. [1]
Clinical picture and diagnostics[edit | edit source]
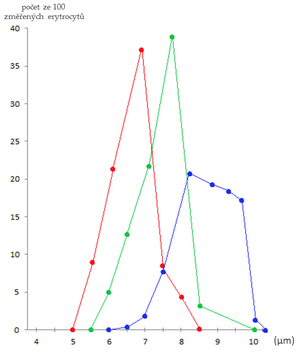
Microcytic hypochromic anemia. Erythrocyte volume distribution (RDW) tends to be increased due to anisocytosis. Thrombocytosis is relatively common (500-700 × 109 / l). [1]
- Prelatent sideropenia - storage iron deficiency (reduced ferritin level, other values in the norm);
- Latent sideropenia - deficit of stored and stored in macrophages. This leads to iron deficiency in erythropoiesis (decreased levels of ferritin, iron and increased soluble transferrin receptor sTFR), without anemia;
- Sideropenic anemia - storage and erythrocyte iron deficiency results in decreased hemoglobin, hematocrit, decreased mean erythrocyte volume (MCV), decreased erythrocyte hemoglobin (MCH) content. It also manifests itself in low levels of iron, ferritin and an increase in overall binding capacity by stimulating transferrin production in the liver and increasing sTFR. Transferrin saturation drops below 16%, hepcidin levels fall. [1]
There is a reduced number of reticulocytes in the blood, there are more erythroblasts in the bone marrow. The marrow is normocellular, hypercellular in anemia due to increased losses. Depletion of storage iron is characteristic (macrophages do not show hemosiderosis). It is manifested mainly by tissue hypoxia (eg tiger heart).
In children, it most often manifests between 6 months and 3 years of age and then at puberty. Iron deficiency during a child's growth can lead to growth retardation, psychomotor development, and cognitive impairment (negative effects on concentration learning). Epithelial damage leads to atrophy of the tongue papillae and increased nail fragility. [1]
Diferencial diagnosis[edit | edit source]
- Anemia of inflammatory diseases - classically normocytic normochromic, in a third of patients microcytic hypochromic, but increased ferritin and hepcidin;
- Thalassemia - microcytic hypochromic anemia, lower RDW, typical target erythrocytes and basophilic erythrocyte spotting;
- Lead poisoning - microcytic / normocytic normochromic anemia; behavioral changes, convulsions, renal damage, abdominal pain and vomiting;
- Sideroblastic anemias - hypochromic erythrocytes, elevated serum iron levels, increased transferrin saturation, crown-shaped sideroblasts in the bone marrow ("wreaths" are mitochondria overfilled with iron). [1]
Therapy and prevention[edit | edit source]
Prevention is the addition of iron to infant formulas, the introduction of meat and vegetable foods, cereals and dairy products enriched with iron, the exclusion of non-adapted cow's milk from infant formulas and the prophylactic administration of iron in premature infants.
Substitution: oral iron preparations (fasting) with concomitant use of ascorbic acid, which increases iron resorption.
Substitution preparations
- Divalent iron salts - ferrous sulphate (Aktiferrin, Ferronat);
- iron complexed with polysaccharides (Maltofer) - fewer side effects;
- parenteral administration of trivalent Fe - with proven malabsorption, significant blood loss, noncompliance, etc. Anemia resolves as quickly as with oral substitution.
Side effects
Feeling of fullness, nausea, constipation or diarrhea. Acute iron poisoning is manifested by severe gastrointestinal symptoms, systemic toxicity. As an antidote, we use deferoxamine, the State Drug Control Authority: deferoxamine, which binds toxic free iron.
The effect of treatment is evaluated by an increase in reticulocytes (4th - 10th day of treatment), a gradual increase in hemoglobin (by 20 g / L in 4 weeks). It usually takes a total of 3-5 months to replenish iron stocks.[1]
Summary video[edit | edit source]
https://www.youtube.com/watch?v=WvD4p8FkQpY
Folic acid and vitamin B12 deficiency anemia[edit | edit source]
- Megaloblastic and macrocytic anemia.
- Folic acid (or its active form - tetrahydrofolate (THF) is essential for DNA synthesis (and therefore for cell division)).
- Vitamin B12 is involved in the conversion of methyl-THF to THF with the simultaneous formation of methionine (important for choline synthesis) from homocysteine.
- Folic acid is found mainly in vegetables, the deficiency begins to manifest itself after several weeks to months.
- The source of vitamin B12 is meat, dairy and egg products, the deficiency only arises after several years.
- Folic acid deficiency affects:
- hematopoiesis - insufficient production of erythrocytes (megaloblastic and macrocytic anemia - predominates), platelets and granulocytes;
- mucosal GIT - Hunter's glossitis, intestinal resorption disorders, diarrhea.
- Vitamin B12 deficiency affects:
- hematopoiesis and mucosal GIT - as vitamin B12 is essential for the proper function of folate, vitamin B12 deficiency can be replaced by folic acid.
- CNS - demyelination of axons, especially in the spinal cord (due to methionine deficiency, which is necessary for choline synthesis, a component of myelin sheath phospholipids), in contrast to anemia, which subsides after the resumption of vitamin B12 supply, neurological manifestations may be permanent;
- homocysteinemia - can lead to thrombosis.
- Castle's antipernic principle.
Castle's antipernic principle[edit | edit source]
- Internal factor - a glycoprotein produced by parietal cells of the gastric mucosa.
- External factor - vitamin B12.
- Vitamin B12 binds to the intrinsic factor, creating a digestion-resistant complex and resorbed by enterocytes in the ileum (they have specific receptors) - the cause of vitamin B12 deficiency is most often a lack of intrinsic factor (gastrectomy, antibodies against intrinsic factor or parietal cells of the gastric mucosa - gastritis A - chronic atrophic gastritis, affects the body and antrum of the stomach) or ileal disease (resection, inflammation, malabsorption, excessive consumption of vitamin B12 by multiplied intestinal bacteria - eg in the intestinal stump after gastrectomy), tapeworm infection Diphyllobothrium latum.
- Vitamin B12 deficiency caused by insufficient dietary intake of vitamin B12 is the most frequently published problem in the vegan diet (the source of vitamin B12 is meat, eggs and dairy products - these foods are not consumed by vegans). Megaloblastic anemia due to insufficient dietary intake of vitamin B12 is very common in developing countries whose people have no money and therefore access to food of animal origin (they become "unwanted vegans").[2]
- Anemia due to an autoimmune process directed against the parietal cells of the gastric mucosa is called pernicious anemia. Autoantibodies destroy parietal cells, the gastric mucosa atrophies, and achlorhydria develops. All this leads to a reduction in the production of intrinsic factor, which is essential for the absorption of vitamin B12 in the ileum. In addition to autoantibodies to parital cells, autoantibodies are also produced that prevent the binding of vitamin B12 to intrinsic factor or prevent the binding of the vitamin B12-intrinsic factor complex to the receptor providing absorption of this complex in the ileum. [3][4]
- Folic acid deficiency leads to folic acid deficiency (eg methotrexate cytostatics - inhibits its conversion in THF).
- The bone marrow is usually hypercellular.
- Marrow cells in the peripheral blood are enlarged (prolonged maturation of their precursors - macrocytes, megaloblasts (large erythroblasts with an immature nucleus)).
- There is more hemoglobin in enlarged erythrocytes (hyperchromic anemia).
- Large erythrocytes often die directly in the marrow without ever circulating (inefficient erythropoiesis) - hemolysis.
- RES macrophages are also increasingly destroyed.
- In addition to the presence of macrocytes, low reticulocyte content and hypersegmentation of granulocyte nuclei are important in the blood count.
Links[edit | edit source]
Related articles[edit | edit source]
- Anemie
- Anemia (pediatrics)
- Hemoglobin
- Hemoglobinopathy
- Hemoptysis, Hemoptoe, differential diagnosis and first aid / PGS (VPL)
- Leukemie
- Vitamin B12
- Vitamin B12 deficiency anaemia
Sources[edit | edit source]
- PASTOR, Jan. Langenbeck's medical web page [online]. [cit. 12.4.2010]. <https://langenbeck.webs.com/>.
Reference[edit | edit source]
- ↑ a b c d e f g h LEBL, J, J JANDA a P POHUNEK, et al. Klinická pediatrie. 1. vydání. Galén, 2012. 698 s. s. 538-540. ISBN 978-80-7262-772-1.
- ↑ NEČAS, Emanuel, et al. Patologická fyziologie orgánových systémů : Část I. 1. vydání. Praha : Karolinum, 2007. ISBN 978-80-246-0675-0.
- ↑ ČEŠKA, Richard, et al. Interna. 1. vydání. Praha : Triton, 2010. 855 s. ISBN 978-80-7387-423-0.
- ↑ JIRÁSEK, Václav, Marie BRODANOVÁ a Zdeněk MAREČEK. Gastroenterologie, Hepatologie. 1. vydání. Praha : Galén, 2002. ISBN 80-7262-139-4.