Thyrotoxicosis
From WikiLectures
Thyrotoxicosis is a condition in which tissues are exposed to high levels of circulating thyroid hormones. The most common cause of thyrotoxicosis is Hyperthyroidism[1], ie excessive thyroid function. Usually in practice, the two terms are often confused.
Etiopathogenesis[edit | edit source]
Hyperthyroidism
- Graves' disease - the most common cause of hyperthyroidism; antibodies against receptors for TSH (TRAK);[2]
- Hyperfunctional goiter
- Hyperfunctional thyroid adenoma - very rare
- Pituitary adenoma secreting TSH - very rare
- Increased secretion of hCG - hCG and TSH are glycoprotein hormones and are partly similar, so at higher concentrations there may be cross-reactivity with TSH receptors, eg pregnancy (mostly at the end of the 1st trimester), hCG-producing mole hydatidosis, testicular tumor
Other (not included in hyperthyroidism)
- Thyroiditis - can cause transient thyrotoxicosis due to the disruption of thyroid follicles by inflammation and the release of stored hormones into the blood. Hypothyroidism usually occurs afterwards. Eg: Hashimoto's thyroiditis, subacute granulomatous thyroiditis, subacute lymphocytic thyroiditis
- Ovarian goiter - ovarian teratoma, producing thyroid hormones
- Thyreotoxicosis factitia - overdose of thyroid hormones or preparations with iodine (contrast agents, amiodaron)
- Neonatal thyrotoxicosis can be caused by transplacental immunoglobulin (TSI) transmission from a mother with Graves' disease.
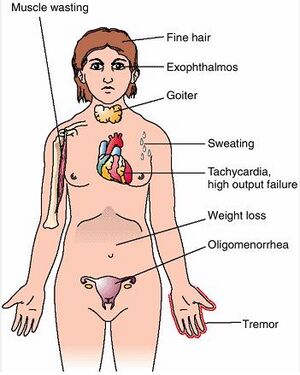
Clinical picture[edit | edit source]
It is caused by a hypermetabolic state and activation of the sympathetic nervous system
- warm, increased perfusion of the skin, excessive sweating, heat intolerance
- weight loss, accelerated growth
- GIT hypermotility and diarrhea
- tachycardia, palpitations, systolic hypertension, large pressure amplitude
- tremor, increased irritability
- thyroid myopathy - weakness of the proximal muscles of the limbs, up to 50% of patients
- exophthalmos (staring expression of the eyes) - caused by the increase of connective tissue due to autoimmune stimulation[3],
- diffuse goiter
- nervousness, motor restlessness, concentration disorders, mood swings
- Graefe's symptom: looking down does not follow the bulbus cap,
- Stellwag symptom: decreased blinking frequency,
- Moebi's symptom: weakened convergence of bulbs.[2]
Diagnostics[edit | edit source]
- Increased T3 and fT4 (the free form of thyroxine, is biologically active and responsible for the tissue effects of the hormone),
- reduced TSH,
- antibodies (against TSH-receptors (TRAK, TRAb, rTSH-ab), thyroglobulin, thyroid peroxidase),
- low serum cholesterol
- Ultrasound of the thyroid gland: volume determination, adenoma diagnosis (+ scintigraphy),
- bone age.[2]
Diferencial diagnosis[edit | edit source]
Treatment[edit | edit source]
- Inicial:
- thyrostatics (block T3 and T4 synthesis) - thiamazole HVLP (Thyrozole), carbimazole or propylthiouracil
- beta-blockers (hyperkinetic circulation)
- Definitive:
- long-term treatment with thyrostatics
- (sub)total thyroidectomy (after repeated relapses after discontinuation of thyrostatics)
- radioiodulation of the thyroid gland by radioiodine ( surgical treatment preferred in the USA)
After TTE (total thyroidectomy) or destruction of the gland by radioactive iodine, the patient usually gradually switches to hypothyroidism with a lifelong need for levothyroxine replacement therapy.
Neonatal hyperthyroidoism[edit | edit source]
- a rare life-threatening disorder
- etiology: transplacental transmission of maternal antibodies against the TSH receptor (TRAb, rTSH-ab) or unrecognized Graves-Basedow-type thyrotoxicosis,
- clinical picture in the fetus: intrauterine growth retardation, fetal tachycardia, acceleration of bone maturation, goiter, exophthalmos,
- clinical picture in untreated newborn: metabolic disruption, heart failure,
- therapy: conservative antithyroid treatment, gradual discontinuation within 2-3 months (maternal antibodies disappear from the circulation).[3]
Links[edit | edit source]
Related articles[edit | edit source]
External links[edit | edit source]
- Hyperthyroidism and ECG - Free ECG book
- Thyrotoxicosis in czech
Reference[edit | edit source]
- ↑ HOLUB, V. Tyreotoxikóza. Postgraduální medicína [online]. 2003, roč. -, vol. -, s. -, dostupné také z <https://zdravi.euro.cz/clanek/postgradualni-medicina/tyreotoxikoza-153007>.
- ↑ a b c MUNTAU, Ania Carolina. Pediatrie. 4. vydání. Praha : Grada, 2009. s. 77-78. ISBN 978-80-247-2525-3
- ↑ a b LEBL, J, J JANDA a P POHUNEK, et al. Klinická pediatrie. 1. vydání. Galén, 2012. 698 s. s. 187. ISBN 978-80-7262-772-1.
Used literature[edit | edit source]
- HAVRÁNEK, Jiří: Tyreotoxická krize.
- KUMAR, Vinay. Robbins basic pathology. 8. vydání. Philadelphia : Saunders/Elsevier, 2007. ISBN 978-0-8089-2366-4.
- PASTOR, Jan. Langenbeck's medical web page [online]. [cit. 2010-05-19]. <https://langenbeck.webs.com/>.