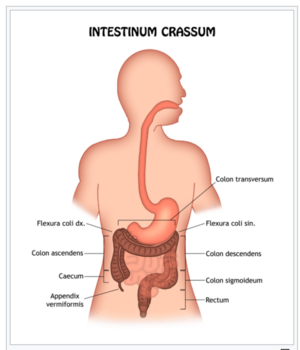
The large intestine
The large intestine (intestinum crassum) is the last part of the digestive tract that receives a mushy to fluid content from the small intestine - chymus . Water and electrolytes are absorbed from chyme in the large intestine. The contents of the large intestine are formed in the stool. The length of the large intestine is 1.2–1.5 m and the width of the large intestine is approximately 4–7.5 cm.
Construction colon wall[edit | edit source]
It consists of 4 layers (histological slides):
- Mucosa of the large intestine
- The mucosa of the large intestine is pale and does not have villi. It is covered by a single layer of cylindrical epithelium. It has numerous glands and long Lieberkühn crypts. It doesn't contain the Paneth cells. The mucosal ligament contains solitary lymphoid follicles (mostly in the appendix). Lymphatic tissue accumulates in the appendix. The lamina muscularis mucosae, which contains both longitudinal and circular bundles, is well formed.
- Submucosal ligament
-
- The colonic ligament of the large intestine is sparse. Contains vascular and nerve plexus and clusters of lymphocytes (nodules) from the mucosa penetrates it.
Large intestinal muscle
- Typical inner circular layer and outer longitudinal layer. The longitudinal layer is very thin, and the circular layer is thickened. Functional sphincters are a local accumulation of circular bundles. It is found in all sections of the large intestine.
Colon serosa
- There is a peritoneal coating on the surface, which is the same as in the small intestine. Creates appendicitis complications - surface protrusions.
Division[edit | edit source]
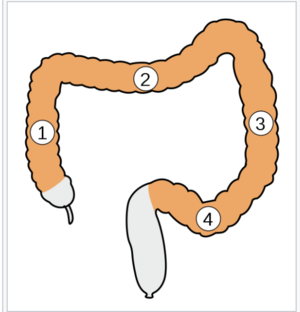
We distinguish the following sections of the large intestine caecum (intestinum caecum, appendix) - the widest part, placed in the right pit of the hip and ileocaecal orifice on the left side of the appendix, appendix vermiformis (worm-like protrusion) - attached to the blind end of the cecum;
- colon ( colon ) - the main part of the large intestine which comprises:
- ascending colon (colon upward) - from appendicitis upward on the right side below the liver ;
- colon transversum (right colon) - from right to left under the liver and stomach to the spleen ;
- descending colon (colon downward) - the left side of the abdominal cavity from the spleen to the left hypogastrium;
- colon sigmoideum (esophageal loop) - from the end of the colon descendens to the center of the small pelvis;
- rectum - the last sections of the intestine in a small pelvis, ends at the opening called the anus. Among the sections of the colon we find typical bends:
- Right colic flexure - under the liver (hepatic flexure - flexura hepatica), between the colon ascendens and the transversum;
- Left colic flaxure- below the spleen (splenic flexion - flexura lienalis), between the colon transversum and the descendens, higher than the right flexion;
- Taeniae coli are 3 whitish longitudinal stripes 8–10 mm wide on the surface of the large intestine, it is a thickening of the longitudinal muscle, according to the position on the transverse colon we distinguish:
- taenia mesocolica - at the back, at the point of attachment to the transverse mesocolon;
- taenia omentalis - anterior upper, at the junction and fusion of the greater omentum;
- taenia libera - front, freely accessible.
- Haustra coli are externally arched places on the intestine, they are a manifestation of the function of the muscle longitudinal (shrinking) and transverse (throttling). By aggregation we denote the action and the immediate appearance of the intestine. On the large intestine, we also find plicae semilunares (crescent-shaped algae) and appendicitis complications , which are protrusions of the serous peritoneal coating of the large intestine, filled with fatty ligament, an unclear function.
- colon ( colon ) - the main part of the large intestine which comprises:
Cecum[edit | edit source]
It forms a sac in the right hip socket, caudally from the ileocaecal orifice (ileum orifice from the left). The length is 6-8 cm, the width is 6-7.5 cm . It rests on the back of the iliacus muscle and the psoas major muscle. The caecum is separated from the fascia muscles by a wall peritoneum, under which the lateral femoral cutaneous nerve runs.
- rectocecal recess - the area behind the caecum, between the intestine and the peritoneum parietale
- ileal papilla (formerly valva ileacaecalis) = a sphincter muscle valve that separates the small intestine and the large intestine
- The junction of the labium superius et inferius in front and behind is called the frenula. The opening allows flow in only one direction - from the ileum to the caeca. This prevents the contents from refluxing.
Appendix vermiformis[edit | edit source]
This is a blind caecum. The length of the appendix is 5-10 cm. The peritoneal duplication, the mesoappendix, which comes to the appendix from the caudal side of the mesenterium of the end of the ileum, serves as a hinge. The appendicular artery passes through the mesoappendix. Ostium appendicis vermiformis is where the appendix opens into the caecum.
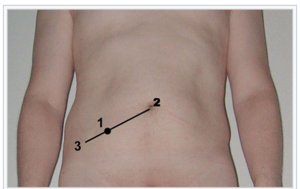
- Lanz point = projection of a part of the appendix on the surface of the abdomen, lies on the linea bispinalis - at the interface of its right and middle third
- McBurney's point = the place where the beginning of the appendix is projected lies on the junction of the superior anterior iliac spine with the navel (linea Monroi), about 6 cm from the spina.
- Appendix positions
- Appendix positions relative to the caecum:
- pelvic position - appendix medially from the caecum, through the linea terminalis extends into the small pelvis (40% of cases);
- retrocaecal position - appendix behind the caecum, heading free end cranially (33%);
- ileocaecal position - medially from the caecum, parallel to the lower end of the ileum (15%);
- laterocaecal position - appendix outside the caecum, cranially free end (2–16%);
- subcaecal position - appendix from caeca ventrocaudally (2–12%);
- paracaecal position - appendix ventrally from the caecum, free end cranially (5%).
- According to another classification, we recognize:
- anterior position - pelvic and ileocaecal position;
- posterior position - retrocaecal and subcaecal position.
During pregnancy, the appendix is gradually pushed out cranially.
The ligamentum appendiculoovaricum is a non-constant peritoneal fold extending from the appendix (in the pelvic or subcaecal position) to the suspension of the right ovary, over the edge of the small pelvis. It is given importance in the spread of disease processes between the two organs, because it connects to lymphatic vessels.
- Appendix wall
- It resembles the wall of the large intestine. The mucosa and submucosal ligament are contain with lymphatic tissue. Therefore, the appendix is often referred to as the so-called "tonsilla abdominalis". The muscle forms a continuous mantle of longitudinal bundles. Three taenias emerge at the caecum from the appendix. There is a serosis on the surface that coats the entire appendix.
Colon[edit | edit source]
It continues from the cecum and wraps around the loops of the small intestine. It passes into a small pelvis in the rectum.
Ascending colon[edit | edit source]
Follows the caecum. On the right side of the abdomen, it points cranially below the liver. It is 12–16 cm long, ie. narrower than the caecum. The transition of the ascending colon into the transverse colon is called flexura coli dextra and lies beneath the liver. Ascending Colon borders: the liver cranially, the right kidney dorsally, the descending duodenum medially and the gallbladder ventromedially. It can be connected to the liver by the hepatocolic ligament or to the gallbladder by the cystocolic ligament. It joins the endoabdominal fascia (covering the iliacus muscle, the Quadratus lumborum muscle), the aponeurosis of the transverse abdominis muscle and the lower pole of the right kidney. Behind the ascendinc colon, the iliohypogastric nerve and the lateral femoral nerve can be found.
Transverse colon[edit | edit source]
Transverse Colon is about 50-60 cm long. It is caudally curved.Left colic flexur is the transition of Transverse colon into descending colon. The spleen is located under the left colic flexture, it is sharper and above the right colic flextur. The transverse colon comes into contact with the liver and gallbladder cranially, the stomach and spleen caudally, the loops of the small intestine dorsally, the anterior abdominal wall ventrally, the duodenum and pancreas dorsally and with both kidneys (during flexures). Transverse Mesocolon (a curtain), shorter on the right (3 cm), longer on the left (10 cm). Left section of the colon transversum more mobile, attachment to the posterior abdominal wall: center of the anterior kidney area → crosses pars descending duodenum and head of pancrease → at the lower edge of the head of pancrease → above flexor duodenojejunalis → anterior renal area (here flexura coli sinistra).
- phrenicocolic ligament - peritoneal, from the left edge of the diaphragm to the left colic flexura , the lower pole of the spleen (from above)
- gastrococolic ligament- part of the greater omentum , between the greater curvatura of the stomach and the Transverse colon - it joins ventrocranially to the taenia omentalis
Descending colon[edit | edit source]
Descending Colon is narrower than the colon transversum (approx. 4 cm), it gradually narrows. The length is 22-30 cm. It descends caudally at the left edge of the abdominal cavity - here it passes into the sigmoid colon. It dorsally associates with symmetrical formations such as the colon ascendens (right). It does not have a mesocolon, fused with the back of the body.
Sigmoid colon[edit | edit source]
The S-shaped last part of the large intestine, leading into the rectum. At the level of the vertebrae S2 and S3, it passes into the rectum. It passes from the descending colon caudally → cranially and medially over the edge of the small pelvis. The crosses behind the peritoneum parietale running through the left common iliac artery , testicular artery (ovarica) and the left ureter → caudally passes into the rectum. The total length is 30-40 cm. This is the narrowest section of the large intestine 3.7 cm. Sigmoid Mesocolon (mesosigmoideum) is a hinge of an S-shaped loop, running in the shape of the letter "N" like a loop. Intersigmoid recession is a deeper, cranial depression between the peritoneum parietale and mesosigmoid at the border of the ascending and last descending part of the mesosigmoid attachment.
Rectum[edit | edit source]
Rectum has two main parts:
- ampulla recti (rectum in the narrower sense) - cranial part, length 10–12 cm, in the range of sacral flexion that passes into perineal flexure .
- anal canal - length 2.5–3.8 cm, narrower, differs in the longitudinal orientation of the mucous membranes.
The construction of the wall of the rectum[edit | edit source]
- Mucous membrane
- It has the same color and appearance as the colon . We find typical mucus and other formations on it.
- In the ampulla recti we find the transverse folds(in the middle of the length of the ampoule), usually three: the upper and lower lashes - rising from the left wall, the Kohlrausch lashing - middle, starting from the right wall.
- anorectalis junction - the border of the ampular part of the rectum and anal canal, it crosses the rectum at the tip of the coccyx.
- In the anal canal we find:
- anal columns - longitudinal lashes, 6-10 pieces around the perimeter of the canal;
- anal sinuses - depressions between the lower ends of the anal columns ;
- anal canals - mucous membranes in the shape of transverse arches, caudally terminating the anal sinuses ;
- rectal epithelium in ampoule monolayer is cylindrical , and has the ability to absorb (suppositories);
- numerous Lieberkühn crypts - a number of goblet cells ;
- anal glands - mucous glands at the site of anal sinus, each of six tubules, opening into the anal crypts, secreting mucus;
- mucosal ligament - contains solitary lymphoid follicles ;
- lamina muscularis mucosae - strong;
- epithelial change during anal canals - single-layered cylindrical epithelium → multilayered squamous non keratinising ;
- pectinate line - a lighter band of the mucosa following the anal sinuses , a multilayered squamous epithelium , the submucosal ligament is denser and stronger.
- Submucosal rectal ligament
- Submucosal connective tissue is high and sparse. The mucosa can move caudally with its weight and with the movement of the contents until it emerges from the anus - the prolapse of the mucosa .
- Rectal muscle
- The outer longitudinal layer is continuous and forms the so-called rectal mantle . All three taenie expanded into the mantle. The circular layer of smooth muscle is reinforced in the upper three quarters of the anal canal, in the range of the zona haemorrhoidalis , anal canals , pectinate line . It forms the internal sphincter muscles , which ends just above the anal margin . The external sphincter muscle, is formed by transversely striated muscle , is attached to the edge of the rectal muscle.
- The surface layer of the rectum
- The peritoneum coats the rectum at the transition from the sigmoid colon, sometimes it form a short mesorectum . Next, the rectum sinks under the peritoneum of the small pelvis. The connection of the peritoneum to the wall of the rectum extends most caudally on the front of the rectum. From there, the peritoneum passes to the urinary bladder in men and to uterus in women .
- This creates deeper hollows of the peritoneum:
- rectovesivalis excavation - in man;
- rectouterina excavation - in a woman (deeper);
- pararectal recesses - slight depressions of the peritoneal wall on the sides of the rectum.
- From the immersion below the peritoneum, the surface of the rectum is covered with a fibrous adventitia (fascia recti) .
Anus - anus [ edit | edit source ][edit | edit source]
This is the external end of the anal canalis . Tough tissue called fascia surrounds the anus and attaches it to nearby structures. The skin is more pigmented, tightened and folded in the radially by the activities of the sphincters. There is no crest in the area of the anus. It is covered by the edges of the buttocks, there are thicker hairs in the immediate vicinity. Circular glands is an apocrine sweat gland forming a ring around the anus. The rigid fibrous plate that connects the wall of the anal canal to the coccyx in the median plane is called the anococcygeal ligment. The mechanism of the anal closure is caused by the sphincters and the pelvic floor muscles .
Internal anal sphincter muscle - enhanced smooth circular muscle of the anal canal, the ring from the anocutanea line cranially to the anal columns .
External anal sphincter muscle- sphincter is made of transversely striated muscle , it encloses the internal anal sphincter muscle from the outside, and attaches itself to the levator ani muscle from below, has three parts:
- Deep part
- The deep component of the muscle that is most cranially. It lies just below the rectal passage through the pelvis diaphragm . The posterior and lateral is in contact with the puborectalis muscle which is part of the pelvic floor ( levator ani muscle ). The medial muscle fibers are circular , and the lateral muscle fibers forming a forward open fork. They are fixed to the urogenital hiatus . Together with the puborectalis muscle, it forms the most important component of the rectal closure mechanism - the functional designation of the compressor recti muscle .
- Superb part
- It consists mainly of circularly arranged fibers anchored at the front to the center of the perineum and at the back to the anococcygeal ligament . The corrugator ani muscle is its functional muscle which is a thin stratum of involuntary muscular fiber, which radiates from the orifice around the anus.
- Pars subcutanea
- It has a subcutaneous ring of muscle fibers. It is fixed by strips of ligament and smooth muscle to the skin around the anus. Its functional component is the corrugator .
M. puborectalis - part of the pelvic floor muscles, recedes on both sides of the symphysis, along the hiatus urogenitalis outside the levator prostatae (puboprostaticus) of a man or pubovaginalis of a woman, surrounds the anal canal at the level of the pars profunda sphincter or externus , creates a musculus compressor recti .
Muscle innervation : pudendus nerve , components from the levator musculus or - directly from the sacral plexus (S 3 –S 4 ).
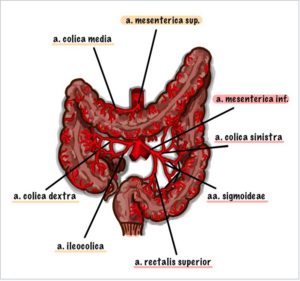
Arteries and veins[edit | edit source]
- Superior mesenteric artery - caecum, ascending colon + trans transverse colon.
- Interior mesenteric artery - transverse colon, descending colon, sigmoid colon, upper rectum.
- Arteria iliaca interna - lower part of the rectum.
- veins of the same name, vena portae + vena cava inferior (anastomosis).
- Caecum
- superior mesenteric artery → ileocolic artery → caecal artery
- appendicular artery
- ileocolic vein
- superior mesenteric vein → vena portae
- Colon
-
- Colon ascendens : superior mesenteric artery → dextra colonic artery
- Transverse colon : inferior + superior mesenteric artery → media and sinus artery
- Colon descendens : inferior mesenteric artery → sinus colonic artery
- superior and inferior mesenteric vein → vena portae
- Rectum
-
- a. inferior mesenteric
- internal pudding artery
- superior rectal, media and inferior arteries
- sigmoid artery
- superior, medial and inferior rectal vein
Lymphatic vessels [ modify | edit source ][edit | edit source]
- from the ileum, cecum, appendix and the beginning of the colon ascendant to: ileocolic lymphoid nodes
- from colon ascendens to: right colic lymph nodes
- from right 2/3 colon transversum to: medial colic lymphatic node
- from the rectum in several directions, to: inferior mesenteric nodes or internal iliac lymphatic node
- from the area of the anal orifice to: superficial inguinal lymph nodes - from them to external iliac lymph nodes
Nerves colon[edit | edit source]
- Parasympathetic fibers
They come from the vagus nerve (the beginning of the large intestine to the middle and left thirds of the colon transversum - Cannon-Böhme point), the splanchnic pelvic nerves and the inferior mesenteric plexus (below).
Sympathetic fibers
They come from ganglia celiac , mesenteric ganglion through the superior , inferior mesenteric ganglion .
Links[edit | edit source]
Related articles[edit | edit source]
- Gallery of histological images - digestive system
- Digestive tract
- Large and small intestine
- Small intestine
Bibliography[edit | edit source]
- ČIHÁK, Radomír – GRIM, Miloš. Anatomie. 2. upr. a dopl edition. Praha : Grada Publishing, 2002. 470 pp. vol. 2. ISBN 80-247-0143-X.