Pulmonary valve stenosis
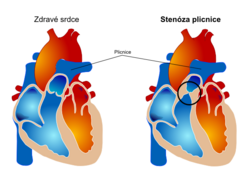
Pulmonary valve stenosis is a rare valve defect in adult cardiology.It can occur alone or as part of a more complex stenosis in the right ventricular outflow tract, mainly the pulmonary area. More generally, pulmonary stenosis refers to both pulmonary valve stenosis and subvalvular or supravalvular obstruction. Diagnosis is based primarily on echocardiographic examination, or catheterization examination to assess pressures.
Etiopathogenesis[edit | edit source]
The most common cause of valvular pulmonary stenosis is a congenital heart defect, where valve stenosis is in most cases part of a complex heart defect such as tetralogy of fallot or complete atresia of the right ventricular outflow tract. However, it can also occur in isolation.
Pulmonary stenosis, as a valve defect, also forms the most common type of stenosis in the outflow tract of the right ventricle, resp. lungs. Pulmonary stenosis as a whole occurs in several forms depending on the location of the stenosis. It can be located below the valve (narrowing of the infundibule of the right ventricle in tetralogy of fallot or ventricular septal defect), at the site of the valve, above it or in the periphery of the pulmonary branches (again it can be part of various congenital heart defects). Stenosis subsequently causes right ventricular hypertrophy, which can lead to dilatation and secondary tricuspid regurgitation and right heart failure.
Other possible etiologies of pulmonary stenosis are post-rheumatic valve disease (rare) or carcinoid disease, in which the serotonin produced causes pulmonary valve fibrosis.
Clinical picture[edit | edit source]
The auscultating finding is an ejection murmur above the pulmonary valve, or a cleft of the second echo. Patients may be asymptomatic or experience nausea, dyspnea, and chest tightness. Critical stenosis in the newborn is a life-threatening cyanotic heart defect (due to a right-left atrial short circuit). At a later age, children tend to have no problems with a minor defect, sometimes with lower performance.
Diagnostics[edit | edit source]
The ECG finding depends on the severity of the stenosis. The finding may be normal, with more severe forms of stenosis showing signs of right atrial overload, right ventricular hypertrophy and generally pathological changes in the right precordial leads (high QR, T-wave inversion, etc.).
No significant changes may be seen on the chest x-ray. In neonates, the right heart border is prominent in the right-left atrial shunt and concomitant tricuspid valve involvement. After that, the changes are noticeable mainly in the more severe degree of pulmonary stenosis, mainly in the sense of poststenotic enlargement of the lung and enlargement of the right lateral compartments.
Echocardiographic examination is the basic examination method for assessing the anatomical abnormalities of the pulmonary valve and the hemodynamic effects of the defect. The examination is not always simple and it is necessary to assess the parameters of the tricuspid valve, including pressure gradients.
Therapy[edit | edit source]
The course is usually benign, a mild defect does not require treatment. Prostaglandin E1 is given to neonates in some specific situations.More severe stenosis can be treated with balloon valvuloplasty or, in the event of its failure, by cardiac surgery..
Links[edit | edit source]
Related articles[edit | edit source]
References[edit | edit source]
- MANN, Douglas L, et al. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 10th Edition edition. 2015. ISBN 978-0-323-29429-4 .
- CZECH, Richard, et al. Internal. 3rd edition. Triton, 2020. ISBN 978-80-7553-782-9 .
- BENEŠ, Jiří. Study materials [online]. © 2009. [feeling. 2009]. < http://jirben.wz.cz >
Reference[edit | edit source]
- ČEŠKA, Richard, et al. Internal. 3rd edition. Triton, 2020. ISBN 978-80-7553-782-9 .
- ↑Jump up to:a b c d e f g h i MANN, Douglas L, et al. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 10th Edition edition. 2015. ISBN 978-0-323-29429-4 .
- ↑Jump up to:a b c BENEŠ, Jiří. Study materials [online]. © 2009. [feeling. 2009]. < http://jirben.wz.cz >.