Psoriasis
Psoriasis (psora = peeling, scratching) is a non-infectious inflammatory autoimmune disease of the skin. It has a chronic course and a tendency to relapse. The most common manifestation is peeling of the skin, as it changes up to seven times more often than normal. The etiology is unclear, hereditary predispositions seem to play a certain role (in up to 30% of patients). Approximately 2% of the population is affected, men and women are equally affected. The disease usually begins between the ages of 10 and 30, uncommon in children under 8 years of age. Difficulties are worse in spring and autumn.
Risk factors[edit | edit source]
- infection – guttate psoriasis following streptococcal angina
- medications – beta-blockers, lithium or antimalarials worsen psoriasis
- exposure to sunlight - mostly improvement after exposure to sunlight, worsening of seeding in 6% of patients
- psychological stress - the same effect as in other chronic skin problems
- smoking, alcohol, refined sugar
Pathogenesis[edit | edit source]
The epidermis is thickened, the keratinocytes contain nuclei, the granular layer is absent, and the keratin in the stratum corneum is loose. The stratum corneum is infiltrated by polymorphonuclear cells that form microabscesses. Capillaries expand and T lymphocytes accumulate.
Clinical pictures[edit | edit source]
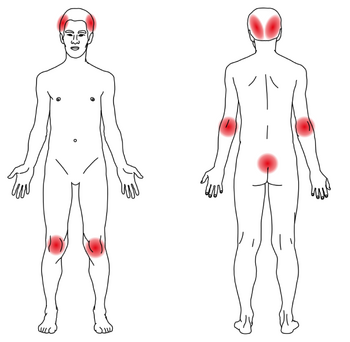
Psoriasis comes in many forms ranging from mild to life-threatening. Appearance varies from classic involvement of elbows and knees to acute generalized pustular form. It most often affects the large joints and extensor sides of the limbs, the scalp (in some patients the only manifestation), nails, but it can appear in any location.
- First, a flat red papule covered with silvery shiny scales, after scratching the papule, these scales bounce off like wax flakes (wax drop phenomenon);
- Auspitz´s phenomenon – with more severe traumatization of the deposit, the capillaries are disrupted, which extend pathologically high into the epidermis, resulting in dot-like bleeding;
- Koebner´s phenomenon – psoriatic manifestations appear at the site of previous trauma.
Forms of psoriasis[edit | edit source]
- Acute exanthematic form – in younger individuals, the symptoms of psoriasis are usually preceded by angina or a virus, then the appearance of papules;
- Psoriasis punctata – seeding of very small papules;
- Psoriasis guttata – teardrop-sized papules;
- Psoriasis nummularis – large papules, up to 1 cm in diameter;
- Chronic stationary form – the predilection places for papules are on the elbows, knees and in the lumbosacral region (places more mechanically stressed), but they can also appear in other places (in the armpits, on the palms and soles, under the nails or in large skin eyelashes), papules they have the same character as in the acute form, but they gradually increase in size, merge and even create geographical configurations, the condition can result in psoriatic erythroderma;
- Psoriasis pustulosa;
- Barber – limited to palms and soles, in middle-aged women;
- Zumbusch – generalized form, severe general symptoms, may result in erythroderma;
- Psoriasis arthropathica – simultaneous severe involvement of small joints.
- Psoriasis flexuralis – affecting the axilla, submammary areas, groin, navel, more common in old age;
- Nail involvement - in 25-50% of patients, nail pitting, onycholysis, oily spots, nail bed hyperkeratosis, more often on DK
Therapy[edit | edit source]
This inflammatory, relapsing to chronic disease requires long-term treatment, which should be chosen individually depending on the type of psoriasis, the extent of the involvement, the patient's age and social background.
- mild to moderately severe form – analogue of vit. D, topical steroids, tar preparations, tazarotene, UVB
- severe forms – UVB / PUVA, methotrexate, cyclosporine, biological treatment
- facial involvement, flexure - topical steroid preparations, tacalcitol
- psor. Barber – strong topical steroids, Acitretin, PUVA
- generalized pustular form and erythroderma – Acitretin, methotrexate, cyclosporine, biological treatment
Analogs of vit. D[edit | edit source]
- calcipotriol, tacalcitol, calcitriol – they inhibit the cell. proliferation, stimulate keratocyte differentiation, well tolerated, no smell, no staining, no risk of skin atrophy
- side effects: local skin irritation, hypercalcemia at high doses, calcipotriol is not suitable for the face and scalp
Topical steroids[edit | edit source]
- hydrocortisone 1%, hydrocortisone-butyrate 0.1%, triamcinolone – weak, moderately effective
- betamethasone, mometasone, methylprednisolone-aceponate, fluticasone – strongly effective
- clobetasol – very strong
- easy to use, no staining, no irritation. The problem is skin atrophy with long-term use. Strong preparations should not be applied to the face.
- there are combined preparations steroid + vit. D analogue (Daivobet)
Tar preparations[edit | edit source]
an effect probably by inhibition of DNA synthesis. The problem is that it smells and stains clothes. Use mainly in hospitalized patients, in combination with UVB.
Anthralin[edit | edit source]
Substance with an antimitotic effect, has an irritating effect on healthy skin, must not be applied to the face and genitals, stains skin, hair, bedding, sanitary equipment. Mostly used in hospitalized patients, application with increasing concentration (from 0.1-2%), the surrounding skin must be protected with Vaseline.
Keratolytics[edit | edit source]
- 5% salicylic acid – for hyperkeratosis of the palms and soles
- 3% salicylic acid – for the brush, in combination with tar shampoo (Polytar)
Systemic treatment[edit | edit source]
- methotrexate – in severe disease or forms resistant to topical therapy, in arthropathy. Dosage 7.5–15 mg once a week. Contraindications and side effects as with other methotrexate use.
- acitretin – a derivative of vit. And, in pustular psoriasis, thinning of hyperkeratotic lesions. Good in combination with UVB – PUVA.
- adverse effects: dryness of the mucous membranes, itching and peeling of the skin, hyperostosis, hyperlipidemia, liver damage, teratogenic.
- ciclosporin – in severe forms, inhibits T-lymphocytes and IL-2 production. Necessary control of blood pressure and renal function, increased risk of cancer or lymphoma. Not suitable for combination with UV.
- hydroxyurea – immunosuppressant, does not affect liver function, but the risk of bone marrow suppression.
Links[edit | edit source]
Related articles[edit | edit source]
References[edit | edit source]
- ŠTORK, Jiří. Dermatovenerologie. 1. edition. Praha : Galén, Karolinum, 2008. pp. 502. ISBN 978-80-7262-371-6.
- Gawkrodger, David, Dermatology. Fourth edition, Churchill Livingstone - Elsevier, 2008, www.elsevierhealth.com