Phosphate
Phosphates:
The total phosphorus content of an adult individual is 700 g. About 85% is contained in the skeleton, the remaining 15% is in the extracellular fluid and soft tissues. We receive 800-1400 mg of phosphorus through food, 60-80% is passively absorbed in the intestine; however, there is also active transport stimulated by 1,25-dihydroxyvitamin D3.
The reference limits for the level of phosphates are in the range of 0.7-1.5 mmol/l in serum and 15–90 mmol/l in urine.
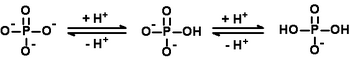
Phosphate anions play an important role in maintaining Acid-Base balance. Phosphate is freely filtered in the glomerulus, more than 80% is reabsorbed in the proximal tubule, a smaller amount in the distal tubule. Proximal reabsorption takes place as passive cotransport with N+.2 different Na–P transporters have been proven to exist. Cotransport is regulated primarily by P intake and further by parathyrin. Acute adaptation to a low or high P supply is accompanied by an increase or, conversely, a decrease in Na–P transport protein molecules in the brush border of the renal tubules. Chronic adaptation to low intake involves increased transporter synthesis in the cell. Parathyrin induces hyperphosphaturia by inhibiting Na–P cotransport, mainly in the proximal tubule. The hormone binds to a specific receptor in the basolateral membrane, which leads to the activation of two intracellular mechanisms: the adenylate cyclase/cAMP/protein kinase A and the phospholipase/Ca/protein kinase C system. One of the very interesting renal effects of phosphate deficiency is resistance to the phosphaturic effect of parathyrin.
Hypophosphatemia[edit | edit source]
Hypophosphatemia is seen in glycolysis-stimulating alkalosis. Phosphate is moved into the cells, where it is used for phosphorylation. Chronic use of antacids that bind phosphates, malabsorption, hypercalcemia and its causes, increased excretion, alcoholism can be the cause. As there is a decrease in 2,3-bisphosphoglycerate in erythrocytes, the binding curve of hemoglobin shifts to the left, thereby impairing the release of oxygen from hemoglobin to the tissues. Symptoms of hypophosphatemia include muscle weakness, articulation disorder, decreased masticatory muscle motility, anisocoria, anorexia, hyperventilation, ATP deficiency, etc.
Hyperphosphatemia[edit | edit source]
Hyperphosphatemia occurs with renal failure, healing of extensive fractures, acromegaly, hypervitaminosis D, increased growth hormone production. In hyperphosphatemia, the amount of calcium ions decreases and calcium-phosphate salts are formed, which are deposited in soft tissues. This can cause serious complications, including acute kidney failure.
Links[edit | edit source]
Related articles[edit | edit source]
Used literature[edit | edit source]
- MASOPUST, Jaroslav – PRŮŠA, Richard. Patobiochemie metabolických drah. 1. edition. Praha : Univerzita Karlova, 1999. 182 pp. ISBN 80-238-4589-6.
- SCHNEIDERKA, Petr, et al. Kapitoly z klinické biochemie. 2. edition. Praha : Karolinum, 2004. ISBN 80-246-0678-X.
- MATOUŠ, Bohuslav, et al. Základy lékařské chemie a biochemie. 1. edition. Praha : Galén, 2010. 540 pp. ISBN 978-80-7262-702-8.