Myocardial infarction (pathology)
Myocardial Infaction (IM, MI, czech heart attack) is ischemic necrosis myocardium resulting from the occlusion of a coronary artery lasting at least 20-40 minutes. It most often arises on the basis of atherosclerotic changes in the coronary artery, which culminate in bleeding into the atherosclerotic plaque or the entrapment of an embolus.
Pathophysiology[edit | edit source]
As a result of cardiomyocyte hypoxia, metabolic changes occur that lead to disruption of their function and subsequently to cell apoptosis or necrosis. Accumulation of some metabolites (lactate, serotonin, adenosine) causes anginal pain in C7–T4 dermatomes. Damaged tissue triggers an inflammatory response. It later heals with a fibrous scar.
An infarcted focus shows impaired kinetics and can lead to a decrease in cardiac output. Cardiac insufficiency can then cause hypertension in the pulmonary basin, which can result in pulmonary edema and dyspnoea, as well as the development of cardiogenic shock. The decrease in systemic pressure activates the autonomic nervous system, which causes increased heart rate, sweating, cold skin, and nausea.
unlike angina pectoris cardiomyocyte necrosis occurs in MI, the pain lasts longer than 15 minutes and does not subside at rest even after administration of nitrates.
Patology[edit | edit source]
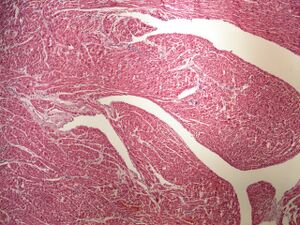
During a heart attack , all the tissue components of the heart muscle undergo necrosis (cardiomyocytes + interstitium) ischemia the necrosis is only partial (cardiomyocytes are necrotized, the interstitium is preserved - tissue that is less susceptible to lack of oxygen) - the so-called myomalacia.
Distribution of myocardial infarction:
- 1. transmural – affects more than 3/4 of the wall, wider than 2.5 cm. It is caused by a thrombotic occlusion of a coronary artery and is localized in the area of its riverbed.
- 2. laminar – affects a certain layer of muscle in the range of 1/3 to 1/2 of the wall, most often it has a subendocardial form. It occurs in severe stenotic sclerosis of most of all three coronary vessels, forming either one continuous deposit or several small deposits.
A transmural heart attack always affects the left ventricle, often together with the septum, because the left ventricle has the greatest workload and therefore also the greatest oxygen consumption. There is also the possibility of simultaneous involvement of the right ventricle and atrial myocardium, but always as part of a deposit extending here from the left atrium. Isolated right ventricular infarction practically does not exist. According to the location of the blockage, we divide transmural infarction into:
- RIA closure – infarction of the front wall (anterior), front wall and septum (anteroseptalis), tip (apicalis),
- RIP closure– infarction of the back (lower) wall (posterior, inferior), back wall and septum (posteroseptalis),
- RC closure– infarction of the lateral wall (lateralis), lateral and posterior walls (posterolateralis).
The most serious is the infarction of the posterior wall, due to the possibility of involvement of the atrioventricular node (from the septi fibrosi of the RIP, in 90% from the right, in 10% from the left coronary artery) - the result of ventricular fibrillation.
Macroscopic appearance of myocardial infarction:
- 18–24 hours – pallor, cyanosis of the myocardium, thinning of the left ventricular wall at the location of the lesion,
- 3-5 days - fully developed coagulation necrosis – yellow deposit with a hemorrhagic rim,
- 1 week – from the periphery, the deposit turns gray (formation of granulation tissue),
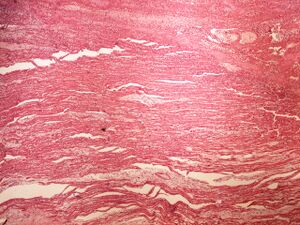
- 6-8 weeks - scarring.
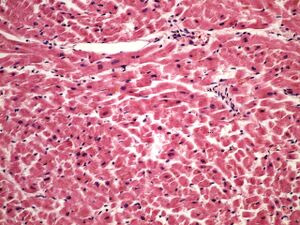
Microscopic appearance of myocardial infarction:
- 4–8 hours – thinning, stretching and undulation of dead cardiomyocytes (due to the pull of the surrounding living muscle), interstitial edema
- 12–24 hours – coagulation necrosis – increase in cytoplasmic eosinophilia, karyolysis (paleness of the nucleus) or pyknosis (shrinking and darkening of the nucleus),
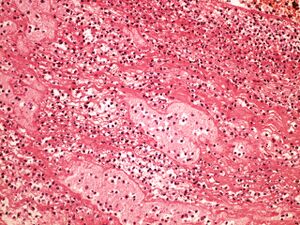
- 24 hours – neutrophils in the vicinity of necrosis (most on day 2-3),
- 3-7 day – breakdown of dead cells, macrophages,
- 7th day – formation of granulation tissue,
- 6 weeks - collagen scar
Complications[edit | edit source]
As part of a kinetic disorder of the myocardium affected by a heart attack and a change in the biomechanical properties, aneurysm, (tissue thickening of the endocardium) may form and organize with possible systemic embolization (brain, kidneys, spleen, intestines, limbs). The wall of the aneurysm consists either of necrotic myocardium (acute aneurysm) or of post-infarction scar tissue, often calcified (chronic aneurysm). ventricular septal defect, mitral valve prolapse due to papillary muscle involvement, functional insufficiency of the mitral valve due to dilatation of the ventricle, perforation of the heart wall and tamponade may occur
- Damage to the left ventricle can lead to left-sided insufficiency and blood stagnation in the lungs, the consequence of which is the development of pulmonary edema.
- Inflammatory response to damage can cause pericarditis - pericarditis epistenocardiaca - fibrinous or serofibrinous inflammation of the pericardium above the focus of transmural infarction or diffuse.
- The infarcted focus prevents the transmission of the action potential, which can be the source of arrhythmias, in the worst case, ventricular fibrillation.
- When blood stagnates in the systemic circulation, a fluidothorax may occur, causing further depression of ventilation.
- Hypoperfusion can lead to hypoxic damage to other organs (kidneys, luungs).
- Rupture of the myocardium – rupture of the free wall of the left ventricle (leads to hemopericardium and cardiac temponade), interventricular septum (formation of left-right shunt) or papillary muscle (mitral insufficiency).
Diagnosis and treatment[edit | edit source]
More detailed information can be found on the Myocardial infarction (internal) page.
links[edit | edit source]
Related articles[edit | edit source]
- Myocardial infarction (internal)
- Infarct
- Angina pectoris
- Biochemical examinations in acute myocardial infarction
- Vascular supply of the heart
- Recommended examination procedure for suspected acute myocardial infarction
- Bypass
- Fresh myocardial infarction (preparation)
External links[edit | edit source]
Source[edit | edit source]
- PASTOR, Jan. Langenbeck's medical web page [online]. [cit. 23.04.2010]. <https://langenbeck.webs.com/>
References[edit | edit source]
- NEČAS, Emanuel, et al. Patologická fyziologie orgánových systémů. Část I. 1. vydání. Praha : Karolinum, 2007. ISBN 978-80-246-0615-6
Kategorie:Patofyziologie Kategorie:Patologie Kategorie:Vnitřní lékařství Kategorie:Kardiologie