Heart rhythm disorders (neonatology)
From WikiLectures
Neonates with arrhythmias may be asymptomatic, may present with heart failure (tachypnea, poor skin perfusion, lethargy, hepatomegaly) or, rarely, collapse. Sometimes arrhythmias are detected prenatally. Tachy or bradyarrhythmias in newborns are usually secondary, arising from non-cardiac pathology. Primary cardiac arrhythmias that would require treatment are uncommon.[1][2]
Sinus rhythm on ECG: each QRS complex is preceded by a P wave, the axis is 0–190° and the PR interval is normal (90–120 ms).[1]
Basic distribution of heart rhythm disorders in newborns:
- Sinus tachycardia' (> 160/min. in full-term and > 180/min. in premature newborns);
- benign causes: temperature stress, pain, drugs (caffeine, catecholamines, atropine);
- pathological causes: fever, shock, hypoxia, anemia, sepsis, open duct of Botall, hypovolemia; rarely hyperthyroidism, cardiac arrhythmias, metabolic disorders and hyperammonemia.
- Sinus bradycardia' (< 80/min. in full-term and < 100/min. in premature newborns).
- benign causes: defecation, vomiting, urination, suctioning of the upper respiratory tract, catheterization, drugs (propranolol, digoxin);
- pathological causes: hypoxia, apnoic pause, convulsions, intracranial hemorrhage, severe hypothermia, airway obstruction, air leak, severe acidosis; rarely hyperkalemia, cardiac arrhythmia, pulmonary hemorrhage, diaphragmatic hernia, hypothyroidism, hydrocephalus.
- Arrhythmia - a consequence of the abnormal formation and conduction of excitation in the heart;
- Tachydysrhythmia:
- Mechanisms:
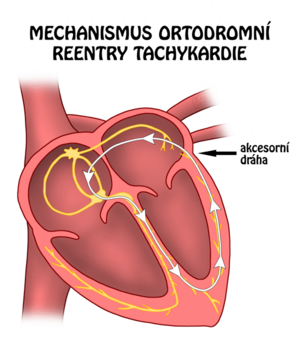
- reentry mechanism (circular excitation)
- triggered activity (abnormal course of repolarization due to ion transport disorder in the wall of cardiomyocytes) or
- abnormal automaticity (spontaneous depolarization in the cells of the conduction system outside the sinus node or outside the conduction system of the heart)
- benign: premature atrial contractions (supraventricular extrasystoles), premature ventricular contractions (P wave absent, QRS complex wide);
- atrial: atrial flutter (rare; atrial rate around 400/min.), atrial fibrillation (very rare), atrial tachycardia (uncommon);
- AV junction: AV reentry tachycardia (common), AV nodal reentry (rare);
- below the AV node: junctional ectopic tachycardia – His bundle tachycardia (very rare, usually postoperative);
- Mechanisms:
- Bradydysrhythmia:
- Tachydysrhythmia:
Diagnosis[edit | edit source]
- 12-lead ECG (speed 50 mm/s, sensitivity 10 mm/1 mV);
- 24-hour ECG monitoring (Holter);
- examination of ABR, electrolytes, inflammatory markers;
- X-ray of the chest, ultrasound of the CNS;
- determination of drug levels that affect heart rate and rhythm.
Treatment[edit | edit source]
- Adenosine
- antiarrhythmic drug; a pure nucleotide that has a negative dromotropic effect on cells of the AV node (with rapid i.v. administration leads to slowing down of AV node conduction); rapidly metabolized by erythrocytes and endothelium; biological half-life 1-5 seconds;
- first aid drug for neonatal supraventricular tachycardia based on WPW syndrome;
- Amiodarone
- Atropine
- parasympatholytic, anticholinergic; indicated for vagal bradycardia;
- Digoxin
- cardiotonic, antiarrhythmic, cardiac glycoside; for the treatment of heart failure with reduced contractility, supraventricular tachycardia, atrial fibrillation and atrial flutter;
- Isoprenaline
- Lidocaine
- Propafenone
- Sotalol
Supraventricular Tachycardia[edit | edit source]
- heart rate 200-300/min. in newborns and infants;
- most often AVRT and FAT in newborns and infants.
Atrioventricular reentry tachycardia (AVRT)[edit | edit source]
- additional atrioventricular coupling - represents one part of the reentry circuit, the other part is the heart's own transmission system;
- most often orthodromic – the ventricles are activated by their own conduction system (slender QRS complex), the atria are activated retrogradely via the accessory coupling (retrograde P wave just after the end of the QRS);
- Wolff-Parkinson-White picture – the accessory coupling is capable of antegrade conduction from the atria to the ventricles → preexcitation of the ventricles via the accessory coupling during sinus rhythm;
- Wolff-Parkinson-White syndrome – WPW picture + AVRT episode;
- mainly in newborns and infants (paroxysms of SVT spontaneously disappear within 1 year of age) and children older than 5 years;
- short episodes are usually well tolerated, attacks lasting hours can lead to the development of heart failure.
Focal (ectopic) atrial tachycardia (FAT, EAT)[edit | edit source]
- abnormal automation of the ectopic focus of the atrial muscle (the P wave has an abnormal shape) → transmission to the ventricles via the AV node;
- very common in newborns and infants;
- episodes are mostly clinically well tolerated;
- small children have a high transfer capacity of the AV node → transfer from atria to ventricles 1:1.
Treatment[edit | edit source]
- vagal maneuvers: immersing the face in ice water (activation of n. X → slowing of conduction and lengthening of the refractory period in the AV node);
- adenosine 0.1-0.3 mg/kg in the form of a fast bolus under ECG monitoring – interrupts the reentry circuit in the area of the AV node;
- with WPW syndrome, it is necessary to have the possibility of external cardioversion (risk of atrial fibrillation with transfer to the ventricles);
- in case of ineffectiveness: propafenone i.v.
- for repeated early relapses: continuous infusion of amiodarone, then oral sotalol;
- rapid atrial stimulation with an electrode inserted through the esophagus;
- synchronized cardioversion (0.5-1 J/kg);
- radiofrequency catheterization ablation (from 5-6 years).[4]Cite error: The opening
<ref>tag is malformed or has a bad name
Atrioventricular block[edit | edit source]
Atrioventricular Block I degree[edit | edit source]
- slowed conduction through the AV node, prolongation of the PR interval > 110 ms' (ie, the norm for newborns);
- asymptomatic;
- causes: idiopathic; VSV eg ASD; myocarditis; digoxin overdose;
- does not require treatment (unless digoxin overdose).Cite error: The opening
<ref>tag is malformed or has a bad name[1]
Atrioventricular block II. degrees[edit | edit source]
- non-transduction of some sinus impulses – not every P wave is followed by a QRS complex;
- Wenckebach type (Mobitz I): PR interval gradually lengthens until after 3 to 6 cycles the P wave is not converted (QRS complex drops out), and this repeats cyclically; it can be a normal phenomenon, e.g. during sleep or anesthesia;
- Mobitz type (Mobitz II): sudden failure of the QRS complex; PR interval is constant - normal or long; The P wave does not conduct intermittently, often at regular intervals;
- causes: VSV (corrected transposition of the great arteries); myocarditis; digoxin overdose;
- treatment of the underlying cause, with Mobitz II individually and possibly pacemaker.Cite error: The opening
<ref>tag is malformed or has a bad name[1]
Atrioventricular block III. degrees[edit | edit source]
- complete AV block; complete interruption of sinus impulses to the ventricles; P waves and QRS complexes are completely dissociated;
- atrial frequency is normal, responsive; the ventricular rate is between 40 and 80/minute; at a rate of ventricles < 60/min. is the risk of heart failure;
- causes: immunological disease of the mother (IgG antibodies against Ss-A/Ro and Ss-B/La in the fetus damage the development of the transmission system – fibrosis of the bundle of His); myocarditis; cardiac surgery; VSV (corrected transposition of the great arteries);
- treatment: pacemaker; acutely: isoprenaline (increases heart rate).Cite error: The opening
<ref>tag is malformed or has a bad name[1]
Notes[edit | edit source]
AVRT & AVNRT (video)
Atrial fibrillation (video)
Atrial flutter (video)
AV block (video)
Related Articles[edit | edit source]
- Heart rhythm disorders • Arrhythmias (pediatrics) • Bradyarrhythmias and bundle branch blocks • Antiarrhythmics
- Heart failure_(neonatology)
- Electrocardiography • Description of ECG • Prophenomena of disturbances in the generation and conduction of excitation on the electrocardiogram
External links[edit | edit source]
References[edit | edit source]
- ↑ a b c d e f RENNIE, JM, et al. Textbook of Neonatology. 5. edition. Churchill Livingstone Elsevier, 2012. pp. 661. ISBN 978-0-7020-3479-4.
- ↑ a b GOMELLA, TL, et al. Neonatology : Management, Procedures, On-Call Problems, Diseases, and Drugs. 7. edition. Lange, 2013. pp. 343-351. ISBN 978-0-07-176801-6.
- ↑ JANOTA, Jan – STRAŇÁK, Zbyněk. Neonatologie. 1. edition. Praha : Mladá fronta, 2013. pp. 42-52. ISBN 978-80-204-2994-0.
- ↑ KUBUŠ, Peter. Poruchy srdečního rytmu u dětí. Pediatrie pro praxi. 2014, y. 15, vol. 4, p. 216-221,
Used literature[edit | edit source]
- RENNIE, JM, et al. Textbook of Neonatology. 5. edition. Churchill Livingstone Elsevier, 2012. ISBN 978-0-7020-3479-4.
- GOMELLA, TL, et al. Neonatology: Management, Procedures, On-Call Problems, Diseases, and Drugs.. 7. edition. Lange, 2013. 343-351 pp. ISBN 978-0-07-176801-6.
- JANOTA, Jan – ZBYNĚK, STRAŇÁK, et al. Neonatology. 1. edition. prague:Mladá fronta. 2013. 42-52 pp. ISBN 978-80-204-2994-0.
- KUBUS, Peter. Heart rhythm disorders in children. Pediatrics for practice. 2014, year 15, vol. 4, pp. 216-221,