Gliomas of the brain
Gliomas are intracranial tumors. They originate from the brain´s own tissue, which is why they are also referred to as intrinsic. Because of its frequent occurence, it belongs to the most important tumors of the CNS. A typical image is a hemispheric tumor growing infiltratively. Even with a relatively large size, it does not dislocate the brain tissue. The lenght of history of symptoms is "inversely proportional" to malignancy.
Classification[edit | edit source]
Tumors from the brain parenchyma are referred to as intrinsic. The vast majority are gliomas (tumors from glia). Tumors from neurons are rare, becauses neurons no longer divide after birth (it is during cell division that malignant transformation can occur) and create a permanent structure necessary for the preservation of memory traces.
Gliomas are further differentiated into:
- astrocytomas,
- oligodendrogliomas,
- ependymomas,
- gangliogliomas.
Clinical manifestations[edit | edit source]
Gliomas (and intracranial tumors in general) are accompanied by a typical triad of symptoms:
- focal neurological deficit,
- intracranial hypertension syndrome,
- secondary epileptic seizures.
Bearing neurological deficit[edit | edit source]
Focal neurological deficits are terminal neurological symptoms that vary depending on the location of the tumor. These are paresis, visual field disorders, mental alteration, disorders of symbolic function (aphasia, dyscalculia),cerebellar symptoms, and cranial nerve function disorders.
Causes of focal neurological findings:
- direct damage to brain tissue by a tumor (permanent),
- peritumorous edema (reversible),
- local compression (not always reversible).
Intracranial hypertension[edit | edit source]
Causes of intracranial hypertension in intracranial tumors:
- intrinsic tumor volume;
- peritumorous edema;
- obstruction of theb cerebrospinal fluid circulation.
Secondary epileptic seizures[edit | edit source]
Secondary epileptic seizures are irritative focal symptoms. An epileptogenic focus is the result of partial damage to neurons at the site of the tumor. This is so called secondary epilepsy, having an organic cause, is also referred to as lesional epilepsy. More often, epilepsy arises if the tumor grows in a certain location. Patients with a tumor damaging the sensory or motor gyrus are most likely to develop epilepsy and mediotemporal structures. It also depends on individual seizure alertness, that is, each individual has a different predisposition to developing epilepsy. Seizures are initially localized (Jacksonian epilepsy), later generalized (grand mal), where the patient´s life is threatened by brain hypoxia and subsequent accentuation of edema around the lesion. An epileptic seizure can often be the first symptom of an intracranial tumor.
Astrocytoma[edit | edit source]
Astrocytoma is the most common glial intracranial tumor, although it can also accur in the spinal cord (especially in children) [1]. Both benign and malignant forms are known. In astrocytic tumors, there is a typical tendency to degenerate from more benign to more malignant forms – benign astrocytomas are often diagnosed in younger patients, and malignant ones in older patients. [2]

Oligodendroglioma[edit | edit source]
Oligodendroglioma is in most cases a benign tumor, but there are also semimalignant forms. It typically affect adult patients, the most common localization is the frontal lobe [3]. The prognosis is more favorable compared to astrocytomas, although the probability of recurrence is still very high [4].
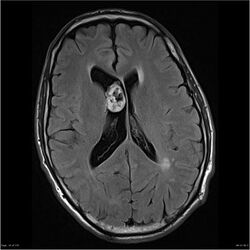
Ependymoma[edit | edit source]
It is a tumor with a relatively diverse biological behavior, there are both benign and malignant forms. Most often, ependymomas grow intracranially in the ventricular system (especially the IV. ventricle), but they can also occur in the spinal cord (they represents 60 % of all spinal intramedullary tumors). Intracranial ependymomas are more common in children, while spinal ependymomas are more common in adult patients. [5][6]
Ganglioglioma[edit | edit source]
Ganglioma is a rare CNS tumor, most often located in the temporal lobe [7]. It is not purely a glioma - it consists of glial and neuronal (ganglion) cells, with the proportions of its components varying in individual patients. In the vast majority of cases, it is a low-grade tumor, although there is also an anaplastic form with highly aggressive behavior and an unfavorable prognosis [8]. It mainly affects younger patients [9].
Links[edit | edit source]
Related articles[edit | edit source]
- Meningiomas
- Astrocytoma
- Glioblastoma
- Oligodendroglioma
- Ependymoma
- Schwannoma
- Vestibular Schwannoma
- Spinal tumors
- CNS tumors (pediatry)
Source[edit | edit source]
- BENEŠ, Jiří. Studijní materiály [online]. ©2007. [cit. 2009]. <http://www.jirben.wz.cz/>.
Used literature[edit | edit source]
- ZEMAN, Miroslav, et al. Speciální chirurgie. 2. edition. Praha : Galén, 2004. 575 pp. ISBN 80-7262-260-9.
- ARNAUTOVIĆ, Kenan – GOKASLAN, Ziya. Spinal Cord Tumors. - edition. Springer, 2019. 540 pp. ISBN 9783319994383.
Reference[edit | edit source]
- ↑ KEPES, J J, C M STRIEBINGER a C E BRACKETT. Gliomas (astrocytomas) of the brain-stem with spinal intra- and extradural metastases: report of three cases.. Journal of Neurology, Neurosurgery & Psychiatry. 1976, roč. 1, vol. 39, s. 66-76, ISSN 0022-3050. DOI: 10.1136/jnnp.39.1.66.
- ↑ ROBINSON, Clifford G., Richard A. PRAYSON a Joseph F. HAHN. Long-term survival and functional status of patients with low-grade astrocytoma of spinal cord. International Journal of Radiation Oncology*Biology*Physics. 2005, roč. 1, vol. 63, s. 91-100, ISSN 0360-3016. DOI: 10.1016/j.ijrobp.2005.01.009.
- ↑ JOHNSON, D.R., F.E. DIEHN a C. GIANNINI. Genetically Defined Oligodendroglioma Is Characterized by Indistinct Tumor Borders at MRI. American Journal of Neuroradiology. 2017, roč. 4, vol. 38, s. 678-684, ISSN 0195-6108. DOI: 10.3174/ajnr.a5070.
- ↑ OHGAKI, Hiroko a Paul KLEIHUES. Population-Based Studies on Incidence, Survival Rates, and Genetic Alterations in Astrocytic and Oligodendroglial Gliomas. Journal of Neuropathology & Experimental Neurology. 2005, roč. 6, vol. 64, s. 479-489, ISSN 0022-3069. DOI: 10.1093/jnen/64.6.479.
- ↑ MALDJIAN, Joseph A. a Rita S. PATEL. Cerebral neoplasms in adults. Seminars in Roentgenology. 1999, roč. 2, vol. 34, s. 102-122, ISSN 0037-198X. DOI: 10.1016/s0037-198x(99)80025-x.
- ↑ CHAMBERLAIN, Marc C.. Ependymomas. Current Neurology and Neuroscience Reports. 2003, roč. 3, vol. 3, s. 193-199, ISSN 1528-4042. DOI: 10.1007/s11910-003-0078-x.
- ↑ RUMBOLDT, Zoran, Mauricio CASTILLO a Benjamin HUANG, et al. Brain Imaging with MRI and CT : An Image Pattern Approach. - vydání. Cambridge University Press, 2012. 433 s. ISBN 9781139576390.
- ↑ SONG, Jye Young, Jeong Hoon KIM a Young Hyun CHO. Treatment and Outcomes for Gangliogliomas: A Single-Center Review of 16 Patients. Brain Tumor Research and Treatment. 2014, roč. 2, vol. 2, s. 49, ISSN 2288-2405. DOI: 10.14791/btrt.2014.2.2.49.
- ↑ LOUIS, David, Hiroko OHGAKI a Otmar WIESTLER, et al. WHO Classification of Tumours of the Central Nervous System. - vydání. International Agency for Research on Cancer, 2016. 408 s. ISBN 9789283244929.