Examination of endothelial damage
From WikiLectures
- Endothelial damage – mechanical, toxic, viral, oxidative and other effects (homocysteine),
- atherosclerosis – a diverse combination of changes in the arterial intima that results in local accumulation of lipids, other blood components and fibrous tissue, accompanied by changes in the vascular wall medium,
- 2 hypotheses: lipid hypothesis and vascular endothelial damage hypothesis,
- lipid triad – high LDL, low HDL and triacylglycerolemia.
Total cholesterol[edit | edit source]
- A very serious risk factor for atherosclerosis, with its increasing concentration the risk increases exponentially (norm 3.5–5.2 mmol/l).
Lipoproteins[edit | edit source]
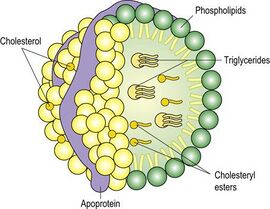
- Blood lipids bound to protein transporters, their structural core consists of non-polar triacylglycerols and esterified cholesterol, the shell consists of polar molecules, ie phospholipids, free cholesterol and apoproteins.
Apoproteins[edit | edit source]
Chylomicrons[edit | edit source]
- They are formed in the small intestine, have the largest volume, contain the most lipids, therefore have the lowest density, transport exogenous cholesterol and triacylglycerols from the intestine,
- lipoprotein lipase on the endothelial membrane cleaves triacylglycerols from chylomicrons, the resulting fatty acids serve as an energy source for muscles and other tissues, the rest is stored in adipose tissue or is taken up by the liver and converted back to triacylglycerols,
- chylomicrons without triacylglycerols containing mainly cholesterol are rapidly removed from the circulation liver.
VLDL (very low density lipoproteins)[edit | edit source]
- They are formed in the liver, where they receive endogenous triacylglycerols and small amounts of cholesterol, then flushed into the blood, where they take over more cholesterol from HDL and are cleaved by triacylglycerol endothelial lipoprotein lipase.
IDL (intermediate density lipoproteins)[edit | edit source]
- They are taken up by the liver and largely metabolized, the rest is converted in the liver by liver lipase (it cleaves their remaining triacylglycerols) to LDL.
LDL (low density lipoproteins)[edit | edit source]
- The main cholesterol-transporting lipoproteins, whose core contains practically only cholesterol esters, bind to the receptors of cells of various tissues and deliver cholesterol to them, the remaining LDL are taken up and metabolized by the liver,
- cholesterol in the cell after LDL binding – becomes part of the cell membrane or is reesterified and stored as storage cholesterol,
- cholesterol in the hepatocyte after LDL binding – excess cholesterol is excreted in the bile in the form of bile acid.
HDL (high density lipoproteins)[edit | edit source]
- They are formed in the liver and small intestine, are the smallest, receive free cholesterol from cell membranes, esterify it and transport it in the nucleus, cholesterol then passes on to VLDL, which enters the liver,
- prevents atherosclerosis (removes cholesterol from cells to the liver and prevents oxidation of LDL particles).
Atherosclerosis[edit | edit source]
- LDL penetrates the damaged endothelium (hypertension, smokers) into the intima of the arteries, where LDL binds to the intercellular mass (glycosaminoglycans), followed by free radicals or aldehyde binding (glucose glycation in DM or malondialdehyde formed by the action of free radicals on fatty acids in LDL) on the amino group of lysine apoprotein (apoB-100),
- glycooxidation – simultaneous glycation and action of free radicals, thus creating highly reactive AGE - compounds (advanced glycation end products),
- 1. stage of atherosclerosis – altered LDL particles are absorbed in the vessel wall by macrophages after binding to scavenger receptors, which then change into so-called fatty cells,
- 2. stage of atherosclerosis – further accumulation of cholesterol destroys the foam cells and releases cytokines and growth factors, which cause the proliferation of vascular smooth muscle and ligament, thus forming a fibrous plate,
- 3. stage of atherosclerosis – fibrous plaque calcifies, it can rupture and form a thrombus attached to the atherosclerotic plaque.
Examination[edit | edit source]
- Cholesterol concentrations in HDL and LDL (HDL cholesterol and LDL cholesterol), total cholesterol alone has no informative value, as it is only the sum of cholesterol contained in LDL and HDL particles,
- AI (atherogenic index) = total cholesterol / HDL-cholesterol,
- concentrations of apoA-1 (contained in HDL) and apoB-100 (contained in LDL), the apoB-100 / apoA-1 index is measured, the higher the index, the higher the risk of atherosclerosis,
- lipoprotein A – has a similar structure as plasminogen, thus preventing the binding of plasminogen to fibrinogen (antifibrinolytic effect), in addition it supports the proliferation of smooth muscle cells, acts independently of LDL and other risk factors for atherosclerosis,
- homocysteine – in hyperhomocysteinemia (an inherited metabolic defect) there is a rapid development of atherosclerosis and increased blood clotting, probably by damaging the endothelium or shortening the life of platelets,
- T - folic acid is given (coenzyme needed to convert homocysteine, it is converted to methionine),
- fibrinogen – promotes platelet aggregation, thus increasing blood viscosity, binding lipoproteins and supporting the proliferation of vascular smooth muscle, the concentration of fibrinogen increases significantly in smokers,
- microalbuminuria – an important predictive factor for cardiovascular disease, because it points to increased endothelial permeability (even large vessels such as coronary or cerebral)
- PCR (polymerase chain reaction) – evidence of familial hypercholesterolemia (a defect in the production of LDL receptors on cells, LDL circulates increasingly in the blood).
Disorders[edit | edit source]
Hyperlipidemia[edit | edit source]
- Hypercholesterolemia – an isolated increase in total cholesterol (mainly LDL fraction).
- Combined hyperlipidemia – increased cholesterol and triacylglycerols.
- Hypertriacylglycerolemia – isolated increase in triacylglycerols.
Links[edit | edit source]
Related articles[edit | edit source]
Literature[edit | edit source]
- SCHNEIDERKA, Petr. Kapitoly z klinické biochemie. 2. edition. Praha : Karolinum, 2004. ISBN 80-246-0678-X.
Portal:Clinical biochemistry
Portal:Cardiology
Portal:Pathobiochemistry
Portal:Internal medicine