Classification of pneumonias (pathology)
Pneumonia is evaluated causally according to the causative agent, and according to the anatomical-pathological classification we assess whether it is alveolar (surface), or interstitial inflammation.
Alveolar (superficial) pneumonia[edit | edit source]
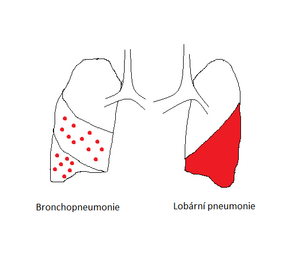
These include lobar pneumonia and bronchopneumonia. The etiology is either aerogenic or, more rarely, hematogenous transmission of pathogenic agents and descending bronchogenic transmission of inflammation. The main complications are empyema, lung abscess, sepsis or ARDS.
Lobar pneumonia[edit | edit source]
It is also referred to as croupous or fibrinous pneumonia. Characteristics:
- involvement of the entire lung lobe or segment;
- S. pneumoniae is an almost exclusive agent;
- development from full health;
- Hight fevers;
- four morphologically distinguishable stages of the course (inflammatory congestion, red hepatization, gray hepatization, resolution).
Bronchopneumonia[edit | edit source]
They are characterized by both descending bronchogenic development and separate deposits (up to 4 cm). These initially develop in the lower parts of the lung lobes and may confluent in later stages. Unlike lobar pneumonia, foci are not in uniformly characteristic phases of the course of inflammation.
Interstitial pneumonia[edit | edit source]
They are defined by the course in the alveolar septa.
Non-purulent interstitial pneumonia[edit | edit source]
Infectious interstitial pneumonia:[edit | edit source]
- Acute = caused by the obligate pathogen, healing or transition to chronic form may occur
- Chronic = with the gradual development of symptoms of other diseases (eg pulmonary fibrosis)
Their pathological representation varies according to the pathogenic agent.
Non-infectious forms:[edit | edit source]
- Idiopathic = no demonstrable origin and non-infectious nature
- Allergic = caused by the ingress of organic dust into the alveoli and the induction of type III hypersensitivity reaction.
Idiopathic interstitial pneumonia (IIP)[edit | edit source]
The older name is "cryptogenic fibrotic alveolitis", which suggests that it typically leads to pulmonary fibrosis. It is divided into several types:
- common interstitial pneumonia (fibrotization with lymphatic tissue accumulation);
- desquamative interstitial pneumonia (accumulation of macrophages in the alveoli with first-order pneumocyte detachment);
- lymphocytic interstitial pneumonia (massive inflammatory cellulitis of the septum);
- bronchiolitis obliterans with interstitial pneumonia.
Hypersensitivity pneumonitis (extrinsic fibrotic alveolitis)[edit | edit source]
It is often associated with a work history. It occurs in acute, subacute and chronic forms. Examples:
- farmer's lung (allergen = thermophilic Actinomyces in moist manure);
- disease of pigeon breeders (allergen = proteins in bird droppings);
- brewers' disease (allergen = Aspergillus clavatus' 'in rotting malt).
Decaying interstitial pneumonia[edit | edit source]
These are lung abscess and pulmonary gangrene. Decaying pneumonia has various origins and arises mainly as one of the complications of pneumonia.
Links[edit | edit source]
Related links[edit | edit source]
Sources[edit | edit source]
Bibliography[edit | edit source]
- POVÝŠIL, – ŠTEINER, Ivo. Speciální patologie. 2. edition. Praha : Galén : Karolinum, 2007. 430 pp. pp. 111-115. ISBN 978-80-246-1442-7.
- KRAHMS, Matthias. Kurzlehrbuch Pathologie. 2. edition. Stuttgart. 2013. pp. 185-189. ISBN 978-3-13-143252-0.