Biochemical indicators of acute myocardial infarction
Acute coronary syndromes (ACS; acute myocardial infarction, AMI, and unstable angina pectoris) are usually caused by coronary artery occlusion due to thrombotic complications. When blood flow is restricted, "myocardial ischemia" occurs, which is initially "reversible". If it is not possible to restore the blood flow in time, "irreversible" changes occur after about an hour, accompanied by the death of cells and necrosis (definitive myocardial infarction).
Laboratory investigation methods play an important role in the diagnosis of acute coronary syndrome. Biochemically important components of the cardiomyocyte are found ``in the cytoplasm or mitochondria and others are part of the ``contractile apparatus. During a myocardial infarction, they are released into circulation. The course of their serum levels is dependent on several factors:
- on localization in the cell;
- During ``short-term ischemia, ``cytoplasmic proteins are washed into the blood circulation as a result of functional and later also structural changes in cell membranes.
- With "longer-term ischemia" tissue necrosis develops and "structural proteins" are also released into the bloodstream. Thus, cytosolic proteins are released faster than structural proteins.
- on relative molecular weight – smaller proteins are released into the circulation faster;
- on the rate of excretion – smaller molecules are eliminated faster by the kidneys;
- on blood flow in the affected area.
| Component | Mr [Yes] | Biological half-time |
Localization in the cell |
|---|---|---|---|
| Creatine Kinase (CK) | 86 000 | 17 h | cytoplasm |
| • isoenzyme MB (CK-MB) | 86 000 | 13h | |
| Lactate dehydrogenase (LD) (mainly isozyme LD1) |
135 000 | 110 h | |
| Myoglobin | 17 800 | 15 min | |
| Cardiac troponin T (cTnT) (cytoplasmic fraction) |
37 000 | 2–4 h | |
| Cardiac troponin I (cTnI) (cytoplasmic fraction) |
22 500 | 2–4 h | |
| Cardiac troponin T (cTnT) | 37 000 | 2-4 h | fibrillar contractile complex |
| Cardiac troponin I (cTnI) | 22 500 | 2–4 h | |
| Aspartate aminotransferase (AST) (mitochondrial isoenzyme) |
93 000 | 34 h | mitochondria |
| Parameter | Start of level rise [h] | Peak levels [h] | Normalization [days] | Maximum level increase [times the upper limit of normal values] |
Normal values |
|---|---|---|---|---|---|
| Myoglobin | 0.5–2 | 4–10 | 0.5–1 | 20× | M 19–92 μg/l F 12–76 μg/l |
| CK mass' | 2–6 | 12-24 | 2–3 | 0.0-5.0 μg/l | |
| CK-MB' | 3–6 | 16–36 | 3–5 | 25× | M 0.2–3.6 μkat/l[tab2 1] Ž 0.2–3 ,1 μkat/l |
| cTnT | 3–8 | 12-18 (1st peak) 72-96 (2nd peak) |
7–14 | 300× | 0.00-0.05 μg/l |
| cTnI | 3–12 | 12-24 | 5–10 | 0.0-0.1 μg/l | |
| AST' | 4-8 | 16–48 | 3–6 | 25× | 0.05-0.72 μcat/l |
| LD' | 6–12 | 24–60 | 7-15 | 8× | 3.5–7.7 μcat/l |
- ↑ The upper limit depends on the age – the indicated values are for the age of 40–50 years.
Cytoplasmic proteins
Myoglobin
Myoglobin is a globular protein consisting of a single chain of amino acids that contains heme as a prosthetic component . It reversibly binds and transports oxygen in muscle cells. Myoglobin from skeletal muscle and myocardium is identical . In the kidneys, it is filtered through the glomerular membrane and excreted in the urine. It has a very short biological longevity, 10-20 minutes.
Unlike hemoglobinmyoglobin contains only one heme group and one globin chain, and therefore can transport only one O 2 molecule . The affinity of myoglobin for oxygen is higher compared to hemoglobin . [3]
As a low molecular weight cytoplasmic protein, it is very quickly released from the affected tissue. Elevated serum myoglobin levels in acute myocardial infarction (AMI) begin rapidly (0.5–2 hours) from the onset of chest pain. Myoglobin levels, which can reach 20 times physiological levels, peak in about 6-12 hours and return to baseline within 12-24 hours. Myoglobin is considered to be the most sensitive biochemical marker of acute myocardial infarction suitable for early detection . The disadvantage of myoglobin determination in AIM is the lack of cardiospecificity . Its increase can be observed:
- any skeletal muscle damage (including eg intramuscular injections or minor bruising after a fall),
- after a large muscular load (including, for example, engaging the abdominal press during prolonged vomiting),
- in renal insufficiency.
Myoglobin determination may rule out an acute myocardial infarction: if it is certain that the blood was taken outside the diagnostic window, ie more than 2 hours after the onset of chest pain or other symptoms, and if serum myoglobin is within the reference range, the diagnosis of acute infarction is myocardial infestation. If myoglobin is positive, it is necessary to differentially consider the reason for its increase (myocardium, skeletal muscle, renal insufficiency) and it is usually necessary to evaluate more specific cardiomarkers - troponin or CK-MB mass.
Various immunochemical methods are used for the determination (immunoturbidimetry, immunonephelometry, enzyme immunoassays, rapid immunochemical tests).
Creatine Kinase
Lactate dehydrogenase
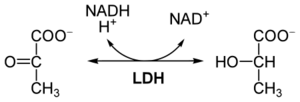
Lactate dehydrogenase ( LD or LDH , EC 1.1.1.27)is an redox enzym that catalyzes the reversible conversion of lactate to pyruvate . The structure of the molecule consists of 4 subunits with a relative molecular weight of 34,000. Each of these subunits can be either M ( muscle ) or H ( heart ), so there are a total of 5 isoenzymes called LD 1 (with subunit composition H 4 ) to LD 5 (M 4 ). LD is present in the cytoplasm of many tissue cells. It is released into the circulation even with mild tissue damage.
| isoenzyme | subunits | occurrence |
|---|---|---|
| LD 1 | H 4 | myocardium + erythrocytes |
| LD 2 | H 3 M | myocardium + erythrocytes |
| LD 3 | H 2 M 2 | skeletal muscles |
| LD 4 | HM 3 | liver + skeletal muscles |
| LD 5 | M 4 | liver + skeletal muscles |
Examination
An increase in the catalytic concentration of total LD in the serum accompanies a number of diseases. Currently, the determination of total LD activity is used as a non-specific marker of cell lysis, eg in cancer ( leukemia , testicular tumors). A late increase in total LD after myocardial infarction , which can last for up to 15 days, is also characteristic. Due to the high erythrocyte content, haemolysis may falsely increase serum concentrations . The use of LD and its isoenzymes for the diagnosis of acute coronary syndrome is now considered obsolete.
The physiological upper limit of LD for adult men and women is 4.10 µkat / l.
An optical test is used for the determination . The presence of isoenzymes can be determined electrophoretically .
Mitochondrial proteins
Aspartate aminotransferase
Aspartate aminotransferase' (AST) is contained in the myocardium in a relatively high concentration. Historically, it was one of the first used biochemical indicators of acute myocardial infarction, but today it is no longer recommended for this indication.
Structural proteins
Troponins
Troponin T (TnT) and troponin I (TnI) are used as cardiomarkers. TnT and occur are found in skeletal muscle and myocardium. Cardiac isoforms (cTnT and cTnI) have a unique amino acid composition and are therfore specific to the myocardium. In most cases, the cardiac isoforms TnT and TnI are contained in the contractile apparatus and are released due to proteolytic degredation. Only 6–8% cTnT and 2.8–8.3% cTnI from the unbound cytosolic component.
Troponin cTnT is not normally present in the blood. The course of cTnT release is biophasic. the increase in troponin after an acute myocardial infarction occurs within 3–8 hours and the first peak is reached 12–18 hours after myocardial injury. It is induced by tge rapid release of the free cytoplasmic fraction of cTnT. The initial peak is followed by another peak in 3–4 days, which corresponds to a slower leaching of cTnT bound in the troponin-tropomyosin complex in the necrotic bearing. It drops to undetectable levels within 7–10 days.
With early resumption of coronary artery blood flow, the maximum rise is about 14 hours, followed by a later second, significantly lower peak. The length of the increase depends on the size of the heart attack. For grater heart attacks, cTnT can be detected for up to 21 days. A disadvantage of cTnT is its non-specific increase in patients with renal insufficiency.
The onset of elevated cTnI levels, which is characterized by high specificity, occurs similarly to cTnT about 3 hours after the onset of ischemia. Elevated levels persist for 5-10 days. Compared to cTnT, no second maximum (smaller cytosolic fraction) is usually observed for cTnI.
Troponin C (TnC) is not suitable for the diagnosis of acute coronary lesions because it is identical in heart and skeletal muscle.
Troponins are determined by sensitive immunochemical methods.
Rapid test for cTnT
Acute myocardial infarction requires rapid diagnosis, which may include the use of biochemical tests to determine myoglobin and troponins, which can be performed at the patient's bedside.
We will describe a rapid test for the determination of cardiac troponin T, based on GLORIA technology (Gold Labelled Optically Read Immuno Assay) by Roche. It uses two different monoclonal antibodies against cTnT – one is labeled with biotin, the other with colloidal gold.
- Preforming the test
The patient's blood is applied to an application zone containing labeled antibodies, which form a sandwich complex with the troponin molecules in the sample (if present) in the reaction zone . Before entering the detection zone, the erythrocytes are separated using glass fibers and only the plasma containing the immunocomplexes proceeds. In the detection zone there is a signal strip with anchored sterptavidin (protein with high affinity for biotin) and another control strip with immobilized troponin. An excess of gold-labeled antibodies bind to the control strip. The color of the control strip confirms that the test is functional and the test is valid. The troponin sandwich immunocomplex is captured by streptavidin, which is indicated by the second colored band. In a positive test, therefore, 2 stripes develop - in the area of the control and signal lines, in the case of a negative result, we observe only the colored control line.
Links
Related Articles
- Biochemical examinations in acute myocardial infarction
- Myocardial infarction
- Ischemic heart disease
References
- ↑ ZIMA, Tomas, et al. Laboratory diagnostics. 1. edition. Prague : Galén, 2002. 728 pp. ISBN 80-7262-201-3.
- ↑ SEAGULL, Jaroslav, et al. Clinical Biochemistry. 1. edition. Prague : Galén – Karolinum, 1999. 316 pp. pp. 176. ISBN 80-7262-023-1.
- ↑ ŠVÍGLEROVÁ, Jitka. Myoglobin [online]. The last revision 2009-02-18, [cit. 2010-11-12]. <https://web.archive.org/web/20160416224337/http://wiki.lfp-studium.cz/index.php/Myoglobin>.