Basic and advanced cardiopulmonary resuscitation
Basic emergency resuscitation[edit | edit source]
This article is about resuscitation of adults. Resuscitation of children is discussed in the article Cardiopulmonary resuscitation (pediatrics) .
Basic Life Support ( BLS ) is a set of knowledge and skills needed to ensure and maintain a free airway and support circulation and breathing, without the use of special aids and medications intended for resuscitation, or the use of an automatic defibrillator , which is already available in many places. Even a trained layman is able to provide basic emergency resuscitation. It must be started when one of the three basic vital functions (consciousness, breathing, heart activity) is impaired. While for breathing and heart activity we only evaluate whether it is preserved in the affected person or not, for consciousness it is necessary to be able to distinguish between two states - fainting and unconsciousness .
It is based on the recommendations of the ERC (European Resuscitation Council 2010) and ILCOR (International Liaison Committee of Resuscitation).
Incidence[edit | edit source]
- Sudden Cardiac Arrest is the leading cause of death in adults in Europe. 80% of these cases have a cardiac cause, most often based on ischemia . Approx. 10% have a cause in another internal disease and the remaining 10% have other causes such as: intoxication, trauma, suicide attempts. [1]
- About 25-30% of cardiac arrests from a cardiac cause begin as ventricular fibrillation or pulseless ventricular tachycardia, but this percentage is thought to actually be as high as 60%. This deviation is caused by the unavailability of ECG measurements in the field directly at the rescue site.[2] If basic emergency resuscitation is provided in this period (ventricular fibrillation, pulseless electrical activity), the percentage of rescue is the highest.
Chain of Survival[edit | edit source]
It represents the ideal procedure and sequence of actions that increase the survival rate of patients with circulatory arrest. It includes all actions from the recognition of cardiac arrest to the activation of the medical emergency service to the hospitalization of the patient in the intensive care unit. As with any chain, its strength depends on its weakest link.
Links in the chain of survival
- Early recognition of cardiac arrest and its cause. Do not delay calling the emergency medical service. Important especially in cases where the cause of the arrest is ischemia of the heart muscle - activation of emergency services already when chest pain occurs, even before the onset of cardiac arrest, accelerates the transport of the patient and the subsequent catheterization examination of the heart and coronary arteries.
- Early initiation of urgent cardio (pulmonary) resuscitation , even by untrained laypersons, right at the scene of the accident until the arrival of emergency medical services.
- Timely use of an automatic defibrillator if available. The use of a defibrillator within five minutes of the arrest (in the phase of ventricular fibrillation or ventricular tachycardia - shockable rhythms) increases the probability of survival to 49-79%. Conversely, every minute lost before defibrillation reduces the chance of survival by 10-15%.
- Early initiation of extended cardiopulmonary resuscitation and transport to hospital and post-resuscitation care including therapeutic hypothermia.
Performing Basic Emergency Resuscitation (BLS)[edit | edit source]
When we arrive at the patient and before starting basic emergency resuscitation , we always follow the well-known rule of Airway Breathing Circulation .
BLS algorithm[edit | edit source]
Security check[edit | edit source]
We make sure that there is no danger when trying to reach the rescued person, or that the rescued person is not threatened by any other external danger (fire, water, etc.) before starting resuscitation.
Checking the consciousness of the rescued person[edit | edit source]
Determining consciousness consists of several steps, where we first rule out sleep and then possible fainting. We find out whether the patient responds to being addressed or to physical contact (slight shaking of the shoulder). To distinguish unconsciousness from deep sleep, it is necessary to induce a painful stimulus. We use pressure on the parotid gland, which is sensitive to palpation due to the branching of the facial nerve. We place the tips of the index and middle fingers above the angulus mandibulae and press them together. We can also indicate a movement as if we wanted to run our fingers behind the ramus mandibulae. If a person fainted, he should react to this painful stimulus by moving his facial muscles. If there is no reaction, we assume unconsciousness.
- If there is no response - call for help, turn the affected person on his back (carefully - watch out for cervical spine injury), check if the airways are open (slightly forward the lower jaw);
- recognizing the obstruction and clearing the airway is key to the next step in emergency resuscitation.
Ensuring free airways[edit | edit source]
We will perform a revision of the oral cavity. Then comes the tilt of the head. This is because if we tilt the head back before the revision, the obstruction would fit into the laryngopharyngeal area and cause obstruction. We check whether the patient is breathing (excursion of the chest, airflow coming out of the mouth, breathing movements and accompanying sounds), whether breathing is normal (regular), irregular (gasping, etc.) or not at all. This check should not take more than 10 seconds. When in doubt as to whether breathing is normal, act as if it were pathological.
- If breathing is normal, we observe the patient and call the emergency medical service (155 or 112). We do not move the patient unless necessary. Maintained breathing is defined as a condition where the affected person breathes at regular intervals and the ventilating air has the same volume. Conditions where there are noticeable pauses between breathing cycles, or when the affected person does not breathe for a long time and then takes a deep breath in and out, are not considered breathing.
- If breathing is abnormal or absent, we will send for help - call the emergency services and, if necessary, provide an automatic defibrillator (if there are more rescuers) or, in the case of one rescuer, we will try to contact the medical emergency service ourselves by mobile phone and start immediate resuscitation. We do not leave the patient unless absolutely necessary.
- Procedure for relieving airway obstruction
- Mild obstruction of the airways : the patient can speak, cough, breathes.
- Severe airway obstruction : the patient is unable to cough, does not respond, gasps for breath, cannot breathe, is unconscious. We check the oral cavity, if no foreign body causing obstruction is visible and the patient still shows signs of obstruction, we place one hand from the front on the chest and by hitting the other hand between the victim's shoulder blades, we try to release the obstruction and allow coughing. If blows do not help, we perform the so-called Heimlich maneuver . The rescuer stands behind the patient and wraps his arms around the epigastrium, pushing sharply towards him and upwards (craniodorsally). If even this maneuver does not help to open the airways, we start immediate resuscitation.
Initiate emergency resuscitation[edit | edit source]
The decision-making mechanism is discussed in detail in the article Principles of starting and ending emergency resuscitation
We also start resuscitation if the affected person shows no breathing movements. We take a position next to the patient, preferably kneeling, place the edge of the palm of one hand in the middle of the patient's chest (lower half of the sternum), place the other hand above the first, check the position of the hands and, with outstretched arms, begin chest compressions. Compression should be up to 1/3 of the depth of the body . After each compression, there should be a complete release of pressure, but without losing hand contact with the patient's chest. We perform compression at a frequency between 100-120 per minute , to the rhythm of the song Jingle Bells or Stayin' Alive. The ratio of chest compressions and breaths into the victim is 30:2. We open the patient's mouth and plug the nose, bend the head and exhale into the patient's mouth. At the same time, we monitor the inspiratory movement of the chest. We relax the mouth and watch the exhalation. This is how we do two breaths. The breaths are gradual, the volume of inhaled air into the affected person is about 0.5 l, which is about the ventilating air during calm breathing. During these two breaths, we stop chest compressions. These two breaths should not last more than five seconds. After their execution, we repeat the whole cycle again. We do not interrupt resuscitation and check the pulse unless the patient himself regains consciousness.
"Compressions only" resuscitation[edit | edit source]
According to the new recommendations, it is no longer necessary to breathe into an adult in any case. The theory is that most causes of unconsciousness in an adult are cardiac in origin. If an arrest occurs, the person becomes unconscious, but still has oxygenated blood in the vascular bed. Therefore, artificial respiration is not necessary, but indirect cardiac massage would only take place without breaks, at a frequency of 100/min. However, this method is not self-saving. According to studies, the saturation sufficient to deliver oxygen to the cells drops after 4-5 minutes. After that, "compressions only" resuscitation slowly loses its effect. However, the philosophy is that it is better to do at least something than nothing at all. We also only perform chest compressions without artificial breaths if we are not trained or for reasons of personal safety are not willing to perform artificial breaths.
Interruption of resuscitation[edit | edit source]
- Arrival of professional help (medical emergency service);
- when handing over resuscitation to another rescuer;
- when the rescuer or rescuers are completely exhausted;
- restoration of vital functions in the patient.
Failure to initiate resuscitation[edit | edit source]
- In case of danger to the rescuer;
- in the presence of certain signs of death (post-mortem spots, post-mortem stiffness, post-mortem putrefaction);
- if the victim has injuries incompatible with life;
- in the terminal stages of an incurable disease.
Use of an automatic defibrillator[edit | edit source]
AED is now found in places with an increased concentration of people (airports, shopping centers, sports stadiums, exhibition centers...). If there are more people doing resuscitation, someone bystander should go for the AED, definitely do not interrupt the CPR. Timely use in the phase of ventricular fibrillation can save the patient's life. The automatic defibrillator will instruct you on how to use it.
Algorithm of using an automatic defibrillator[edit | edit source]
- We make sure that there is no external danger to the patient or the rescuers;
- we proceed according to the emergency resuscitation algorithm by checking the patient's consciousness and ABC;
- in the case of multiple rescuers, one initiates emergency resuscitation according to the above-mentioned algorithm, the other of the rescuers notifies the rapid rescue service and transports the automatic defibrillator to the victim;
- in the case of one rescuer, if an automatic defibrillator is in the immediate vicinity of the patient, we will use the automatic defibrillator after notifying the emergency medical services.
- As soon as an automatic defibrillator is available, we glue the electrodes of the defibrillator, we put the defibrillator into operation. With multiple rescuers, we do not interrupt chest compressions;
- then we proceed according to the instructions of the defibrillator, which first analyzes the heart rhythm;
- If a shock is indicated, we must make sure that no one is touching the patient, then press the shock button on the defibrillator.
- After applying the shock, we continue resuscitation with a ratio of chest compressions: artificial breaths of 30:2 and proceed according to the instructions of the defibrillator.
- If shock is not indicated, we continue resuscitation with a ratio of chest compressions: artificial breaths of 30:2 until the arrival of medical help.
Algorithms for BLS in graphic form
Advanced Emergency Resuscitation/SŠ (Nurse)[edit | edit source]
| This article is intended for students of secondary and higher vocational schools
Please do not make factual edits if you do not have the necessary qualifications. Edit with discretion. Discuss material change first in the discussion . |
ALS - advanced life support - extended emergency resuscitation, which is carried out by a medical professional using drugs, aids and special procedures = provision of professional first aid. Cardiopulmonary resuscitation (CPR) is indicated for loss of consciousness when normal breathing is not present.
Procedure for extended emergency resuscitation[edit | edit source]
Performed by medical personnel.
- Assess the situation, the quality of consciousness (addressing, shaking); a life-threatening bleeding condition.
- Open the airway by tilting the head.
- Check breathing (hear, see, feel), it should not last more than 10 seconds.
- Use a defibrillator as quickly as possible, evaluate the ECG curve , pulseless ventricular tachycardia and ventricular fibrillation are indications for shock delivery.
- Deliver the 1st shock (monophasic defibrillator 360 J, biphasic defibrillator 150-200 J).
- CPR 30:2 (frequency 100–120 per minute, depth 5–6 cm) + ensure airway, also ensure entry (in the field 2 attempts then io); duration 2 minutes.
- Assess ECG, deliver 2nd shock (monophasic defibrillator 360, biphasic defibrillator 200–360 J).
- KPR 30:2 + also ensure entry.
- Assess ECG, deliver 3rd shock (monophasic defibrillator 360, biphasic defibrillator 200–360 J).
- CPR 30:2 + adrenaline 1 mg + amiodarone 300 mg.
- Assess ECG, deliver 4th shock (monophasic defibrillator 360, biphasic defibrillator 200–360 J).
- CPR 30:2 + amiodarone 150 mg (pulseless ventricular tachycardia and ventricular fibrillation).
- Adrenaline every 3-5 minutes.
- We continue CPR + defibrillation + drug administration.
- If we evaluate the ECG as a non-fibrillatable rhythm ( asystole, pulseless electrical activity ), we administer Adrenaline IMMEDIATELY as soon as we secure iv (io) entry!
A – airway → patency of airways[edit | edit source]
- This step involves clearing the airway.
- Manual examination of the oral cavity.
- Head tilt.
Aids ensuring the patency of the airways[edit | edit source]
- Air passages (oral, nasal).
- Endotracheal intubation with a laryngeal tube , performed by a doctor.
- Combination tube .
- Laryngeal mask .
- Coniopuncture - when intubation is impossible and other aids fail.
<mediaplayer> https://www.youtube.com/watch?v=sc4BEJLefjo&feature=youtu.be </mediaplayer>
- Part of securing the airways should be CO 2 monitoring . CO 2 is the first value responding to the restoration of blood circulation – it responds by rising.
B – breathing → breathing[edit | edit source]
- Securing the airway should not delay CPR.
- The volume that we breathe into an adult is about 500 ml of air (7-9 ml/kg), I use my own normal breath.
Aids used for artificial respiration[edit | edit source]
How to hold an AmbuVak mask
- Resuscitation mask - increases the safety of the rescuer.
- Resuscitation mask - increases the safety of the rescuer.
- AmbuVak with mask - should have a reservoir and an oxygen supply.
<mediaplayer> https://www.youtube.com/watch?v=V_AhArkj9Lk&feature=youtu.bee </mediaplayer>
C – circulation → circulation[edit | edit source]
- We kneel from the side next to the affected person, who is placed on a solid surface (ideally the ground).
- Place the joined hands on the center of the chest - between the breasts. The upper limbs must be bent at the elbows!
- We compress the chest approx. 5-6 cm deep.
- The frequency of compressions is 100-120 compressions per minute.
- Compression:relaxation = 1:1.
- Aids can be used – Lucas, Autopulse, cardio pump.
- With an effective heart massage, we are able to ensure 30% of the minute cardiac output.
<mediaplayer> https://www.youtube.com/watch?v=hZqwjYPQPbM&feature=youtu.be </mediaplayer>
D – defibrillation → immediate defibrillation[edit | edit source]
Adhesive paddles for defibrillation
- Immediate performance in the treatment of ventricular fibrillation and pulseless ventricular tachycardia.
- Maximum available energy for a monophasic defibrillator (360 J); energy of 150–360 J in a biphasic defibrillator.
- For children, 4 J/kg of energy.
- Possibility of 3 shocks in a row if a medical professional witnesses ventricular fibrillation (monitoring, during catheterization, etc.).
![]() After defibrillation - regardless of the shock result, another resuscitation immediately follows! The assessment of whether an effective rhythm has been restored is carried out after approx. 2 minutes (5 cycles) of resuscitation. → Interruption of the massage for max. 5 s .
After defibrillation - regardless of the shock result, another resuscitation immediately follows! The assessment of whether an effective rhythm has been restored is carried out after approx. 2 minutes (5 cycles) of resuscitation. → Interruption of the massage for max. 5 s .
E – EKG → electrocardiography[edit | edit source]
- ECG rhythm analysis.
- Summation leads (3, 4 or 5 leads) or 12-lead ECG.
- Diagnosis of chin or tachyarrhythmias.
More detailed information can be found on the Arrhythmias Brief Overview/SŠ (Nurse) page .
Cardiac stimulation[edit | edit source]
- Indicated for bradyarrhythmia with impaired consciousness.
- Transcutaneous (transthoracic) × transesophageal × transvenous.
- In the conditions of pre-hospital care, transcutaneous cardio stimulation is used.
<mediaplayer> https://www.youtube.com/watch?v=iKCD73QoqXY&feature=youtu.be </mediaplayer>
F – fluids and drugs → administration of drugs and solutions[edit | edit source]
- O 2 – hyperoxemia is harmful.
- Adrenaline – increases the efficiency of defibrillation, dosage 1 mg even in an adult (0.01 mg/kg) after the 3rd defibrillation.
- Amiodarone – treatment of ventricular fibrillation and ventricular tachycardia, dosage 300 mg after the 3rd cycle, repeatedly 150 mg → 900 mg by infusion for 24 h.
- Application of drugs intravenously or intraosseously, intrabronchial administration of the drug is not recommended.
G – gauging → balance sheet[edit | edit source]
- Consideration of the primary cause, the appearance of the surroundings, the mechanism of the injury.
Reversible causes of heart failure[edit | edit source]
- 4H: hypoxia, hypovolemia, hyperkalemia (hypokalemia, hypocalcemia), hypothermia.
- 4T: tension pneumothorax, cardiac tamponade (including chest trauma), toxic substances (poisoning, overdose), thromboembolic event.
- Accidental hypothermia → extension of CPR.
- Medicines work from 30°C, CPR is performed until TT increases to 35°C.
- Drowning → artificial respiration as soon as possible.
- Hyperthermia → cool, dantrolene in malignant hyperthermia.
- Electro trauma → prolonged CPR, often CNS and myocardial damage.
- Pregnancy → suitable support of the hip up to approx. 15°, equip the fetus within 5 minutes. With subsequent newborn CPR.
- Bronchial asthma → higher energy during defibrillation, longer apneic pauses for easier exhalation.
- Intoxication → what did he eat?, contact the Toxicology Information Center , antidote.
H – human mentation, hypothermia → preservation of brain functions, hypothermia[edit | edit source]
- Preservation of brain functions while maintaining normal flow (50 ml/100g/min.).
- Timely initiation of emergency CPR.
- Oxygen administration.
- Maintaining BP at CNS perfusion value – MAP 60–150 TORR → CPP 50–150 TORR.
- CPP = MAP – ICP (norm. up to 10 TORR)
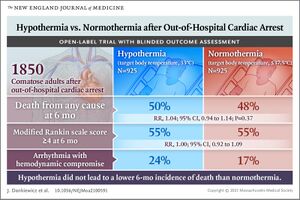
Cooling to maintain normothermia in intensive care after arrest. Currently (2021) the concept of therapeutic hypothermia described below is abandoned. The target temperature is recommended up to 36 °C. Summary infographic Guidelines 2021 and article O. Fraňka ZZS HMP . The following text therefore only describes the methodology of hypothermia.
Therapeutic hypothermia[edit | edit source]
- The indication is non-traumatic circulatory arrest → the aim is to suppress chemical reactions associated with reperfusion trauma – production of oxygen radicals, release of excitatory amino acids, Ca movements → apoptosis, damage to mitochondria.
- It includes administration of cold infusion solutions, application of ice, use of cooling blankets → the goal is to reach a body temperature of 32-34 °C within about 4 hours.
- 4 °C solution in the amount of 30 ml/kg will reduce TT by 1.5 °C.
- Starting already in the ZZS car.
- In acute beds, warm up the patient/client after 24–48 h → 0.5 °C/hour of heating.
- Analgosedation with UPV, in case of muscle tremors, it is possible to administer myorelaxants.
Monitoring[edit | edit source]
- TT needs to be measured continuously and invasively
- Esophageal tube
- Probe in the bladder
- Sensor as part of SG catheter
- Physiological functions – invasive BP, ECG monitoring, GCS, depth of sedation, gases in ASTRUP, CO 2 sensor
Hypothermia does not start[edit | edit source]
- Recurrent cardiac arrest.
- Arrhythmias unresponsive to treatment with worsening P/K status.
- Significant circulatory instability with signs of hypoperfusion.
- Coagulopathy and life-threatening bleeding manifestations P/K.
- An uncorrectable disorder of the internal environment.
Contraindication[edit | edit source]
- Conscious patient/client.
- Terminal state of the disease, a condition precluding the survival of P/K.
- Sudden circulatory arrest (SCA) caused by injury or bleeding.
- Cause of unconsciousness other than NZO.
- Shock with hypotension unresponsive to therapy.
- Pulmonary edema.
- Recurrent ventricular tachyarrhythmias unresponsive to treatment.
- Bradyarrhythmia requiring cardiac pacing.
- Accidental hypothermia.
- Serious immunodeficiency disorders.
I – intensive care → post-resuscitation care[edit | edit source]
- On the dept. ARO, ICU.
- Care of the respiratory tract - UPV.
- Maintaining normotension.
- Trauma solutions, wound care.
- Adequate P/K nutrition.
- Prevention of infection, treatment of septic conditions.
- Rehabilitation.
Post-resuscitation syndrome[edit | edit source]
- The result of ischemia followed by reperfusion of organs with a combination of inflammation and multiorgan dysfunction, injuries caused by CPR.
- Hypoxic encephalopathy.
- Myocardial dysfunction.
- Aspiration pneumonia.
- Ischemic damage to the intestines.
- Renal dysfunction.
- Peripheral limb ischemia.
Pharmacotherapy in emergency resuscitation[edit | edit source]
Pharmacotherapy[edit | edit source]
The article is based on the official recommendations of the American Heart Association Guidelines 2010, which are largely compatible with the European Guidelines 2010.
During resuscitation, pharmacotherapy has the task of increasing blood flow to important organs (heart, brain) and inducing the restoration of circulation (return of spontaneous circulation, ROSC). So far, no clinical trial has shown an increased successful survival in patients where pharmacotherapy was used during resuscitation (although there is a slight positive trend). The main benefit of pharmacotherapy is its positive effect on ROSC, which is sufficiently proven. The pharmacotherapy procedures presented here are general and it should be noted that for specific cases it is appropriate to consider other possible pharmacotherapeutic solutions. The administration of drugs must not result in a delay in indirect cardiac massage.
Possible methods of administration of drugs during emergency resuscitation[edit | edit source]
Intravenous (peripheral) administration (iv)[edit | edit source]
In the field, this is the optimal choice for drug administration. Each dose of the drug should be followed by a bolus of 20 ml of liquid, accelerating its transport to the central riverbed.
See Securing Venous Access for more detailed information .
Central venous catheter[edit | edit source]
Theoretically, it will allow a faster effect of the drug, but it can be a contraindication to fibrinolytic therapy, regardless of the difficulty of its introduction.
See the Central Venous Catheter page for more detailed information .
Intraosseous (IO) administration[edit | edit source]
This method of drug administration is recommended if it cannot be done in the application as well. In this case, the dosage and the effects of the drugs are comparable to iv application.
See the Intraosseous Infusion page for more detailed information .
Endotracheal administration[edit | edit source]
Administration is done through an endotracheal tube. The drugs adrenaline , vasopressin , lidocaine , atropine and naloxone have been demonstrably absorbed through the trachea . The necessary data are not available for amiodarone . In the case of endotracheal administration, the dosage should be increased by 2-2.5x and the dose should be diluted in 5-10 ml of sterile water. Current Guidelines for Cardiopulmonary Resuscitation do not recommend endotracheal administration. Submission also comes to the fore.
More detailed information can be found on the page Endotracheal intubation .
Medicines recommended for routine use in resuscitation[edit | edit source]
Vasopressors[edit | edit source]
- Adrenaline : Vasoconstrictor with an effect on α- and β-adrenergic receptors. It increases the perfusion pressure of the coronary arteries and the perfusion of the brain. Method of administration: iv/io, dose 1 mg every 3-5 minutes.
- Vasopressin : Noradrenergic vasoconstrictor, its effect is comparable to adrenaline. Method of administration: iv/io, dose 40 units.
Antiarrhythmics[edit | edit source]
- Amiodarone: Given for shockable rhythms after the third shock. Method of administration: iv/io, bolus 300 mg (alt. 5 mg/kg), second dose 150 mg.
- Lidocaine : Considered as an alternative to amiodarone if this is not available. It appears to have a positive effect on ROSC. Method of administration: iv, dose of 1 or 1.5 mg/kg, further doses of 0.5-0.75 mg every 5/10 minutes up to a maximum dose of 3 mg.
- Magnesium sulfate: Its use is recommended only in case of torsades de pointes (a rare form of ventricular tachycardia).
Medicines not recommended for routine use during resuscitation[edit | edit source]
- Atropine : A drug previously recommended for PEA bradycardia and asystole. No positive effect on ROSC or patient survival has been demonstrated in clinical trials.
- Sodium bicarbonate: This buffer (and buffers in general) has no proven positive effects, on the contrary, it can lead to intracellular acidosis or can suppress the effect of catecholamines when administered simultaneously. Its use is recommended in special cases (e.g. overdose with tricyclic antidepressants)
- Calcium : Has no clear effects.
- Fibrinolytics : Although initial studies were promising, large studies have not demonstrated the effect of fibrinolytics on the rate of successful resuscitation. Their administration is possible in the event of an arrest caused by a pulmonary embolism .
Therapy for shockable rhythm[edit | edit source]
It refers to ventricular fibrillation (VF) and ventricular tachycardia (VT). The scheme for extended emergency resuscitation is followed . Adrenaline and amiodarone are administered after the third shock and subsequently (dosage and method of administration above).
Therapy for non-shockable rhythm[edit | edit source]
Immediate administration of adrenaline is recommended, amiodarone is not used in this case.
- ↑ BROKMANN, Jörg – ROSSAINT, Rolf. Repetitorium Notfallmedizin. 2. edition. 2010. 393 pp. pp. 118. ISBN 978-3-642-04959-0.
- ↑ VAN ALEM, – VRENKEN, – DE VOS,. Use of automated external defibrillator by first responders in out of hospital cardiac arrest: prospective controlled trial. Britisch Medical Journal. 2003, vol. 327, p. 1312-5, ISSN 0959-8138.