Artificial pulmonary ventilation/SŠ (nurse)
Other articles related to the topic: Introduction to artificial pulmonary ventilation • Artificial pulmonary ventilation (neonatology) • Artificial pulmonary ventilation.
Artificial pulmonary ventilation (UPV) is the basic procedure of organ support. It is a method of breathing in which a mechanical device fully or partially ensures the flow of gases through the respiratory system [1] . The aim of artificial pulmonary ventilation is to support or completely replace the respiratory effort of the patient/client (P/K).
- Long-term UPV → P/K in intensive care beds where basic vital functions fail..
- UPV short-term → P/K in operating theaters undergoing procedures under general anesthesia.
UPV is performed using ventilators. A ventilator is a device that ensures complete or partial exchange of gases between the alveoli and the external environment.
Composition of the pulmonary ventilator[edit | edit source]
Main goals[edit | edit source]
- Ventilation support.
- Support of oxygenation.
- → Support of gas exchange – alveolar ventilation, arterial oxygenation.
- → Influence of the size of the lung volume.
- → Reduction of the patient's work of breathing.
For a purpose:
- → Management of acute respiratory insufficiency.
- → Reversal of hypoxemia.
- → Reversal of acute respiratory acidosis.
- → Prevention of atelectasis and lung redevelopment.
- → Facilitation of anesthesia and sedation, administration of muscle relaxants.
- → Reduction of intracranial pressure.
- → Stabilization of the chest wall.
- → Reduction of oxygen consumption.
- → General anesthesia, analgosedation.
Formy UPV[edit | edit source]
- Positive pressure ventilation → classic ventilation used today.
- Negative pressure ventilation – negative pressure exerted on the chest, no longer used today, formerly the so-called Iron Lung.
- Jet, oscillating, high-frequency ventilation.
Phases of the respiratory cycle on the ventilator[edit | edit source]
- The inspiratory phase = breath – begins with a signal to start the breathing cycle by the ventilator (= triggering) and is limited by limitation (set limits for pressure or volume).
- Inspiratory pause = pause in inhalation – the flow of the mixture in the airways stops, time for gas exchange on the alveocapillary membrane.
- Expiratory phase = exhalation – passive part, given by the elasticity of the chest.
- Expiratory pause = expiratory pause - from the end of the air flow at the end of exhalation to the start of the next breathing cycle.
- Cycling = repeating the breathing cycle, it is done either by volume, time, pressure or flow.
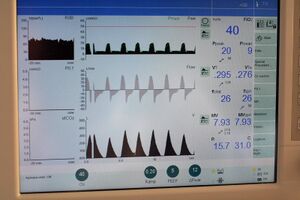
Basic shortcuts[edit | edit source]
- FiO2 = fraction of oxygen – percentage share of O2 in the breathing mixture (21–100% = 0.21–1).
- MV = minute volume – amount of mixture inhaled in 1 min. (MV = Vtxf).
- Vt = volume inhaled in 1 breath (approx. 500 ml).
- PEEP = overpressure value, expiratory brake (in cm H2O)..
- P-peak = airway pressure.
- Total frequency: spontaneous + "artificial" breaths.
- Type of ventilation mode.
- Display of the respiratory curve in graphic form.
Basic fan settings[edit | edit source]
- Tidal volume 5–8 ml/kg id.
- Respiratory rate 12–16/min.
- Inspiratory time 1.2 to 1.5 sec.
- Ratio I:E 1:2 or Ti 33%.
- Pause 10% or 0.2-0.4sec.
- PEEP base 5cm H2O.
- Trigger −0.5 to −1 cm H20 or 3–5 l/min.
- FiO2 0.4; depending on the situation.
- Transpulmonary pressure up to 35 (40) cm H2O.
Positive pressure ventilation[edit | edit source]
UPV, which takes place on the basis of pressure changes in the airways.
We divide it:
- In terms of the patient's respiratory activity:
- Modes ensuring full ventilatory support = ensure the entire breathing work necessary to ventilate the lungs, we also call it SUBSTITUTE ventilation, we set so-called controlled breaths → in patients without respiratory activity.
- Modes ensuring partial ventilation support = for patients who have part of their breathing activity preserved, we include controlled or assisted breathing.
- Assisted breaths - the patient instructs the ventilator with his breathing effort to inhale.
- Modes allowing spontaneous breaths = for patients who must be intubated but have preserved their respiratory activity, can be further distinguished:
- Spontaneous supported breaths - included pressure support.
- Spontaneous unsupported breaths - without pressure support.
- In terms of synchronization:
- Synchronous modes = respect and wait for the patient's breathing effort, synchronization is ensured by triggering → breaths are triggered either by a change in pressure in the circuit or by a change in flow at the end of the expiratory circuit:
- pressure and volume controlled;
- breaths controlled, assisted, spontaneous supported and unsupported.
- Asynchronous modes = the respiratory cycle is initiated regardless of the patient's respiratory effort.
- Synchronous modes = respect and wait for the patient's breathing effort, synchronization is ensured by triggering → breaths are triggered either by a change in pressure in the circuit or by a change in flow at the end of the expiratory circuit:
- In terms of management.
Volume controlled ventilation (VCV, VCA/CMV)[edit | edit source]
- Adjusting the size of the tidal volume → breaths are controlled by the size of the tidal volume.
- Changes in ventilation pressures.
- Indications: initial regimen during times of general instability, apnea, convulsive states, severe dysfunction of the CNS, circulation, breathing, KPCR, status asthmaticus, anesthetic procedures with relaxation, neurosurgical patients.
- Including an inspiratory pause will improve respiratory distribution.
- Allows good control of PaCO2. .
- The size of the inspiratory flow is required to be approximately 4 times the expected minute ventilation - this applies to ventilation with a constant flow.
- Modes include:
- VCV, VC, A/CMV, CMV (controlled mechanical ventilation) → set tidal volume; does not allow you to exercise your own breathing activity;
- SIMV – VC → machine breaths synchronized with the patient's breathing effort, the others are mostly supported by pressure support.
Pressure controlled ventilation (PC, PCV, PC SIMV)[edit | edit source]
- Breaths are controlled by the amount of pressure in the airways, which must not be exceeded during the breathing cycle.
- Variable volumes inspired into the patient.
- There are variants allowing ventilation with non-physiological ratios between inspiration and expiration (PV-IR), where inspiration is equal to or longer than expiration.
- Inspiratory flow of at least 60 l/min is needed to reach the plateau as quickly as possible (it serves the function of an inspiratory pause + aerates closed areas) in order to reach the required level of pressures.
- Better subjectively tolerated.
- Extending the inspiratory time can lead to a better distribution of tidal volume.
- Indications: sometimes preference for patients with lung dysfunction, otherwise generally suitable.
- Unsuitable for patients with convulsive conditions, after CPR, status asthmaticus → for patients with frequent and significant changes in airway pressure.
- Modes include:
- PCV, PC, → variable tidal volume according to changes in resistance and compliance;
- PC-SIMV – synchronized variant.
- A safer variant of UPV due to possible damage from high pressures.
- A certain "self-regulation" of tidal volume at the risk of dynamic hyperinflation → when hyperinflation (end-expiratory pressure) increases, the ventilation pressure gradient decreases → lower tidal volume.
- PSV, PPS, ASB, S/T → spontaneous breaths are supported to the level that is set.
- Necessary breathing activity of the patient.
- PSVG – for children (newborns), volume guarantee; tidal volume (4-8 ml/kg), inspiratory time, Inspiratory Pressure limit (PIP), rate, and PEEP are set → these values are used if the child is apneic.
- The child adjusts his PIP according to improving compliance, reducing it.
Individual modes[edit | edit source]
Pressure-assisted ventilation (PSV, ASB, PPS) = pressure support[edit | edit source]
- The mode with variable tidal volume, when the patient starts the breathing cycle with his effort, the circuit is quickly pressurized and then the pressure is maintained (the ventilator offers the patient a breathing mixture under a certain pressure and makes it easier for him to breathe).
- The aim is to reduce the patient's work of breathing caused by the resistance of the ventilation circuit.
- Indications: patients with the need to ensure DC without ventilatory failure and severe oxygenation disorders.
Synchronized intermittent mass ventilation (SIMV)[edit | edit source]
- It can take the form of pressure- or volume-controlled ventilation.
- It allows three types of breaths - mandatory, assisted and spontaneous.
- Spontaneous breaths are triggered by the patient's breathing effort, the ventilator recognizes them and opens the inspiratory valve.
- Assisted breaths follow the patient's breathing rate and initiate assisted breathing when respiratory effort is detected.
- Mandatory breaths - if the ventilator does not register a respiratory effort during the time window, it initiates a mandatory breath.
- Indication: disconnection from ventilator.
DC continuous positive pressure ventilation (CPAP)[edit | edit source]
- The patient has preserved spontaneous ventilation.
- PEEP is created in the circuit → it keeps exhalation at a higher pressure in DC than the atmospheric pressure.
Biphasic positive pressure ventilation (BIPAP)[edit | edit source]
- The fan switches between two pressure values.
- Possibility of different modes
Fully Controlled Ventilation (CMV)[edit | edit source]
- It can be controlled both by volume and pressure.
- It does not allow the patient to exercise his breathing activity. It is used in patients requiring full ventilatory support.
Hybrid ventilation modes[edit | edit source]
- A mode taking into account multiple control variables
- These include, for example:
- Pressure Regulated Volume Controlled (PRVC) – measures dynamic compliance with each breath, adjusts inspiratory pressure values to achieve volume
- Volume support – modification of pressure support – similar properties to PRVC
- Volume assured Pressure Suport – pressure-controlled mode, there is a guaranteed tidal volume, if the desired tidal volume is not reached at the end of inspiration, a constant flow will replenish the tidal volume
Automatic Tube Compenzation (ATC)[edit | edit source]
- It compensates for the resistance to the flow of the mixture through the cannula → the greater the flow, the greater the resistance.
- The diameter and length of the cannula are entered.
Intricacies in patients on UPV[edit | edit source]
- Limited communication.
- A source of infection that is difficult to locate.
- Don't forget ventilator pneumonia - it hides in effusion, congestion,...
- Don't forget acululous cholecystitis - inflammation of the gallbladder with the risk of perforation.
- Don't forget the risk of sinusitis - in patients with NGS / NJS / NTI!!!
- Ongoing risk of extubation → shallower sedation is advantageous, but there is a risk of self-extubation..
- The advantage is to use sufentanil alone, then propofol for night sedation.
- Combined sufentanil and midazolam only if deep and/or long-term sedation is necessary (craniotrauma).
Sedentary[edit | edit source]
- Adjust the ventilator according to the patient, not the other way around.
- Seated to OTI tolerance.
- The concept of daily interruption of sedation – midazolam + sufentanil.
- The concept of permanent shallower sedation – pure sufentyl.
- The concept with pure sufentanil seems more advantageous.
- The vast majority of patients with TS do not require sedation.
When is tracheostomy better?[edit | edit source]
- The stabilization phase has taken place, longer ventilation support is required.
- When to consider early TS:
- Tachypnea, marginal respiratory mechanics.
- Reduction of R and Vd.
- ET tolerance.
- → High sedation.
- → Conscious patients, intake of food.
- → Striving for articulation/vocalization.
- → Increased mobility.
- Safer DC, suction.
- →Reducing the risk of unplanned extubation.
Links[edit | edit source]
[edit | edit source]
- Overview of airway management
- Intubation – in children
- Endotracheal intubation
- Difficult intubation
- Tracheostomie
- coniotomie
- Laryngospasmus
- Non-invasive pulmonary ventilation/SŠ (nurse)
- Patient/client monitoring at UPV/SŠ (nurse)
- Oxygenoterapie
- PEEP
- Lung Volumes
Links[edit | edit source]
Reference[edit | edit source]
- ↑ Erna Mičudová, Poskytování umělé plicní ventilace v domácím prostředí, Bakalářská práce, Brno, 2006, dostupné on-line
References[edit | edit source]
- DOSTÁL, Pavel, et al. Fundamentals of artificial lung ventilation. 2nd, expanded edition. Prague: Maxdorf Jessenius, 2005. ISBN 80-7345-059-3 .
- Lectures by MUDr. Petra Vojtíška, doctor of ARO Masaryk Hospital in Ústí nad Labem