Sense organs
The cells of the sensory organs have the function of receptors, they receive stimuli from the external environment and the internal organs of the body, which they convert into excitement. Receptors have the ability to convert a sensation (different types of energy – movement, light, chemical substances) into a receptor potential, which triggers an action potential in the sensory nerves. Action potential is carried by nerve fibers (axons) to the CNS, where it is subsequently processed.
Receptors[edit | edit source]
We divide the receptors into mechanoreceptors (including audioreceptors), chemoreceptors and photoreceptors.
Mechanoreceptors[edit | edit source]
- occur as free nerve endings in the skin or as proprioreceptors (endings in muscles, tendons and inner ear)
- perceive muscle tension, joint flexion and body position
Chemoreceptors[edit | edit source]
- found in oral cavity (taste) and nasal mucosa (smell)
- taste cells are arranged in taste cups, which are most often located on the sides of the covered papillae of the tongue
- olfactory cells are found in the upper part of the nasal cavity, pars olfactoria
Photoreceptors[edit | edit source]
- rods and cones in the eye ( sight ), with which we are able to analyze the shapes and intensity of light and colors
- rods are used for night vision, react to lower light intensity, but do not distinguish colors
- the cones are able to distinguish lights of different wavelengths (intensity) and therefore also colors of different saturation
Sensory organ cells[edit | edit source]
The receptor cells of the sensory organs do not have a common origin, and therefore we can divide them into primary and secondary cells. The difference between them is not only in their appearance, but also in the way they transmit information to the CNS.
Primary sensory cells[edit | edit source]
- Primary sensory cells are of neuroepithelial origin (they arise from the epithelium of the neural tube) and, like normal nerve cells, have a sensitive process, by means of which they receive sensations, and a conducting process (axon) that conducts the impulse efferently to the CNS. The primary sensory cells are the rods and cones of the visual apparatus and the olfactory epithelial cells.
Secondary sensory cells[edit | edit source]
- Secondary sensory cells are of ectoderm origin and, unlike primary cells, only have a sensory protrusion. The excitation is carried to the CNS by the fibers of the sensory nerves, they are formed by the axons of the second neuron, whose dendrites are synaptically connected to the axons of the sensory cells. These include the hair cells (ear) and taste bud cells.
Primary and secondary sensory cells are not found alone in the sense organs. In addition to them, there are also supporting, basal and other cells. They have their own functions (support, replacement of dead sensory cells), but they do not include receiving stimuli from the external environment.
Eye[edit | edit source]
The eyeball consists of three layers – tunica fibrosa, tunica vasculosa and tunica nervosa.
Tunica fibrosa[edit | edit source]
The tunica fibrosa is made up of white matter in the back part of the bulb (sclera)and in front by the cornea (cornea)
- sclera – dense collagenous tissue, contains collagen and elastic fibers and elongated, flat fibroblasts
- cornea – transparent and avascular (diffusion nutrition from tunica vasculosa), composed of five layers
- epithelium anterius corneae ( stratified squamous epithelium ) – five to six layers of cells that have the ability to regenerate, thanks to which this epithelium is renewed every 7 days. We also find free nerve endings here. When they are stimulated, the surface of the eyeball is moistened with tears and the eyelids move, all of which is accompanied by sharp pain = corneal reflex.
- lamina limitans anterior ( Bowman's membrane ) – homogeneous layer of collagen fibrils and amorphous mass, serves as BM for the previous layer.
- substantia propria corneae – own stroma of the cornea made of dense collagenous tissue, folded into lamellae. We also find here flattened fibrocytes (keratinocytes) and amorphous matter (chondroitin sulfate). This is the thickest layer of the cornea.
- lamina limitans posterior ( Descemet's membrane) – serves as BM for the following layer and is formed by fine collagen filaments (spatial network).
- endothelium corneale - one layer of flat cells, which are not epithelium (endothelium). It continues to the front layer of the cornea.
Tunica vasculosa[edit | edit source]
Tunica vasculosa consists of three parts, they are :
- choroidea – a layer of sparse collagenous tissue and rich vascularization and melanocytes. It has four layers:
- lamina suprachorioidea – the outer layer (of the sclera) of the HCV with melanocytes.
- zona vasculosa – contains arteries and veins.
- tunica choriocapillaris – the network of capillaries that nourish the retina.
- lamina vitrea (= Bruch's membrane) – a vitreous blank, it is formed by an amorphous hyaline layer and the pigment epithelium of the retina is attached to it.
- corpus ciliare (ciliary body) – it contains smooth muscle m. ciliaris (lens accommodation). The muscle is surrounded by a sparse collagenous tissue with a large number of elastic fibers, melanocytes and capillaries. The surface of the ciliary body is covered by a layer of the retina, the pars ciliaris retinae, which no longer contains light-sensitive cells
- iris ( iris ) – this is a circular projection of the choroid. This projection covers part of the lens and leaves an opening in the middle, the pupil = pupil. It consists of five layers:
- anterior iris endothelium
- anterior boundary layer - here we find the melanocytes that determine the color of the iris
- iris stroma - in this layer we find m. sphincter pupillae of smooth muscle, which is placed concentrically around the pupil and narrows it. Around it is a sparse collagenous tissue with capillaries.
- posterior boundary layer of the iris - here is another muscle m. dilatator pupillae, but it is formed by myoepithelium (muscular epithelium). It goes radially towards the edge of the iris and its task is to dilate the pupil.
- pigment epithelium -single-layered cylindrical epithelium with melanin.
Tunica nervosa[edit | edit source]
The retina (retina) has two parts pars optica retinae and pars caeca retinae. Pars caeca retinae no longer contains photosensitive cells but only a pigment layer and supporting cells and is further divided according to where it is located on pars ciliaris and pars iridis, according to the location on the ciliary body or iris
- Pas optica retinae : 10 layers (from the outermost)
- Pigment epithelium – a single-layer cubic epithelium that sits on the lamina vitrea = Bruch's membrane choroidei. On the opposite side, rods and cones are inserted into the protrusions.
- A layer of rods and cones – their outer parts
- Membrana limitans externa – the projections of Müller cells (belonging to macroglia = supporting cells – nutrition, insulation, strengthening) connect with photosensitive cells here
- Outer core layer – nuclei of rods and cones
- Outer layer plexiform – synapses of rod and cone axons with bipolar cell dendrites
- Inner nuclear layer - nuclei of bipolar and Müller cells
- Inner layer plexiform – synapse of axons of bipolar cells with dendrites of multipolar cells
- The layer of ganglion cells - bodies of multipolar neurons
- A layer of nerve fibers – axons of ganglion cells,they form nervus opticus
- Membrana limitans interna – extended processes of Müller cells
The optic nerve leaves the bulbus in the papilla nervi optici and belongs to the central nervous system, thus it has the same coverings as the brain (dura mater, arachnoid and pia mater). Axons have a myelin sheath formed by oligodendrocytes.
Lens cristallina[edit | edit source]
The lens has a biconvex shape and three layers.
- Capsula lentis ( = case ) – it is firm, flexible and made up of collagen IV and glycoproteins
- Anterior (subcapsular) epithelium – a single layer of cuboidal cells at the front of the lens only, which elongate toward the poles and change into lens fibers without nuclei and organelles.
- Lens fibers – elongated flattened structures of the lens, they connect at the poles and are formed by crystallin proteins.
The lens is attached to the ciliary body by means of a suspension apparatus = zonula ciliaris Zinii.
Lacrimal gland[edit | edit source]
- tuboalveolar serous gland
- numerous myoepithelial cells
- fibrous stroma – abundant infiltration by lymphocytes (lysozyme) and plasma cells (IgA)
- ducts: intralobular (single-layered cubic epithelium) and interlobular (double-layered cylindrical epithelium ) ducts, but no annealed and inserted ducts
- six to twelve ductuli lacrimali open into the conjunctival sac
- function: moistening the surface of the eye, mild bactericidal effec
Lid[edit | edit source]
- inner side - covered by conjunctiva (stratified cylindrical epithelium with goblet cells)
- external side - thin type of skin
- hair follicles - in the free edge of the lid, there is no m. arrector pili
- tarsus – a plate of dense collagen tissue that forms the base of the lid
- muscle - striated muscles orbicularis oculi and levator palpebrae
- glands :
- Meibomian - branched alveolar sebaceous glands located in the tarsus that open into the conjunctival sac
- Zeiss - sebaceous, opening into the eyelash follicle
- Mollovy - apocrine, tubulocoiled
- Krause - accessory lacrimal glands
Nasal mucosa[edit | edit source]

1.bulbus olfactorius,
2.mitral cells,
3.lamina cribrosa,
4. nasal epithelium,
5. glomeruli olfactorii,
6. sensory cells
In the upper part of the nasal cavity, the epithelium of the respiratory tract – multi-rowed cylindrical with cilia and goblet cells (40 – 50 μm) suddenly transitions into multi-rowed cylindrical epithelium (100 μm), in which we find three types of cells.
- Olfactory cells (chemoreceptors) = primary sensory cells - they have 6-8 long specialized cilia apically and their axons go efferently and form the fila olfactoria.
- Supporting cells - cylindrical b., which narrow towards the base and have microvilli on the apical surface.
- Basal (reserve) cells - small pyramidal cells in BM
Fila olfactoria, formed by the axons of olfactory cells, passes through the lamina cribrosa of the ossis ethmoidalis and ends in the bulbus olfactorius. Here, mitral cell dendrites connect to the axons in complex synaptic complexes - olfactory glomeruli, mitral cell axons go to the CNS.
The oral cavity[edit | edit source]
– taste we perceive with taste buds (they are formed by receptor cells), which are located in the oral cavity
- mainly found on the edges of the walled papillae of the tongue (papillae vallatae) - 8 to 12 and form on the tongue in front of the sulcus terminalis (V)
– other locations of taste buds – mushroom and leaf papillae, soft palate, palatal arches, pharynx, plica glossoepiglottica, laryngeal valve
– taste can also be perceived by free nerve endings( sharp taste )
– we recognize five tastes - sweet, sour, salty, bitter, umami (meat, etc.)
Taste bud
- barrel-shaped taste organ
- the taste cells that form it are spindle-shaped and their long microvilli extend into the mucus
- in addition to taste cells, it is also made up of supporting and basal cells
- porus gustatorius – surface pit, forms the entrance to the cup
- on the basal side, the cups are in contact with the dendrites of the neural pathway cells
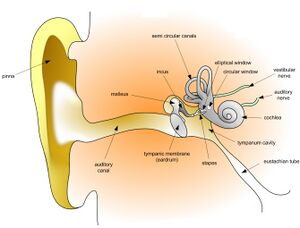
Ear[edit | edit source]
In the inner ear we find balance mechanism ( sacculus and utriculus, semicircular canals ) and hearing system ( snail = cochlea )
Cochlea[edit | edit source]
– formed by a bony and a membranous cochlea
– three spaces here
scala vestibuli ( perilymph )
scala media = ductus cochlearis ( endolymph )
- triangular space between scala vestibuli and scala tympani
- upper limit is membrane vestibularis Reissneri – two-layer flat epithelium ( separates sc. media from sc. vestibuli )
- bottom border – basilaris membrane – the Organ of Corti is located on it
- externally from scala media we find three formations:
- ligamentum spirale cochlae – transformed thickened periosteum of the bony cochlea (three ridges: crista membranae vestibularis, prominentia spiralis, crista mem. basilaris), absorbs endolymph
- stria vascularis – multi-row vascularized epithelium, forms endolymph
- sulcus spiralis externus
- inside - sulcus spiralis internus
scala tympani ( perilymph )
Organ of Corti[edit | edit source]
– organ of hearing placed on the basilar membrane in the scala media
– it is made up of audio receptors and supporting cells
- audioreceptors - hair cells (secondary sensory bb. - only sensory projection) - cylindrical bb., nucleus located basally, stereocilia apically and individual cilia (bending of stereocilia = depolarization), internal (more resistant, less sensitive to sound ) and external (less resistant and more sensitive to sound)
- supporting bb. - hair cells are stored in their depressions
- bb. sulcus spiralis internus
- bb. borderline
- inner phalangeal cells
- pillar cells – between them Corti's tunnel and Nuel's space
- Hensen cells – tall cylindrical
- bb. Claudius - Cubic
- Bötcher's bb. – cubic
- bb. sulcus spiralis externus
- above the hairs of the cells membrana tectoria - a plate made of glycoprotein.
Links[edit | edit source]
Related articles[edit | edit source]
References[edit | edit source]
JUNQUIERA, L. Carlos – CARNEIRO, José – KELLEY, Robert O. Basics of histology. 1. edition. H & H, 1997. 502 pp. ISBN 80-85787-37-7.
LÜLLMANN-RAUCH, Renate. Histology. 1. edition. Grada, 2012. 576 pp. ISBN 978-80-247-3729-4.
BALKO, Jan – TONAR, Zbyněk. Memorix histology. 1. edition. 2016. 0 pp. ISBN 978-80-7553-009-7.