Respiratory tract mucosa
We divide the Respiratory tract into the upper and lower respiratory tract.
Upper respiratory tract[edit | edit source]
We further distinguish parts:
- nasal cavity;
- nasopharynx (pars nasalis pharyngis).
Lower respiratory tract[edit | edit source]
Which include:
- larynx;
- trachea;
- 2 main bronchi;
- secondary (lobar) bronchi for individual lobes;
- tertiary (segmental) bronchi for individual bronchopulmonary segments (10 in the right, 8 in the left);
- bronchiolus terminalis.
Function[edit | edit source]
The main function of the respiratory tract is breathing and oxygen transfer. Other functions include adjusting the humidity of the inhaled air and reducing temperature differences (heating). Furthermore, the air gets rid of larger particles of impurities with the help of the ciliated epithelium. The airways also provide resonance and voice production.
Mucous membrane (tunica mucosa)[edit | edit source]
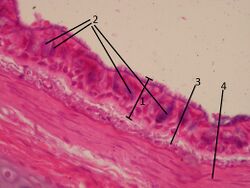
The tunica mucosa consists of the lamina epithelialis and the lamina propria mucosae.
Lamina epithelialis[edit | edit source]
It consists of 'multiple columnar epithelium with cilia. It is characterized by the fact that all cells attach to the basement membrane, but not all reach the surface. Here we find these cells:
- Ciliated cells - work in a coordinated manner within one cell and within the epithelium (they move mucus with impurities). Their cilia oscillate outward, then slowly return. They ensure the self-cleaning ability of the epithelium.
- Goblet cells - produce mucus (glycosaminoglycans = mucopolysaccharides) - more viscous at the surface, thinner at the bottom; captures dirt.
- Basal cells - anchor the epithelium to the basement membrane. They are believed to be stem cells that can differentiate into the missing airway epithelial cells when needed.
- Neuroendocrine cells' - produce serotonin and various peptide hormones. They resemble neuroendocrine cells in the GIT. Their exact function is not yet known, but due to the rich innervation of the cells, it is assumed that they serve as mechanoreceptors or chemoreceptors.
In the section from the nasal cavity to the larynx, the mucosa is partially covered with stratified squamous epithelium, which is mechanically more resistant to friction due to direct air flow.
Lamina propria mucosae[edit | edit source]
In the lamina propria there are venous plexuses' (mainly in the nasal cavity) in which a large amount of blood flows due to their rich blood supply. This causes the flowing air to heat up. On the right and left side, the venous plexuses are filled differently, and air mostly flows through the wider part. In this layer of the mucous membrane, we find seromucinous tuboalveolar mixed glands' that secrete mucin as a respiratory tract secretion. This secretion covers the mucous membrane, prevents it from drying out and at the same time moistens the penetrating air. The serous component contains antibacterial proteins.[1] Cells of the immune system are freely scattered in the lamina propria, and in some places there are also lymphatic follicles (B-lymphocytes and T-lymphocytes).
Mucous membrane differences according to anatomical localization[edit | edit source]
Nasal cavity[edit | edit source]
The skin in the nasal cavity transitions into multilayered squamous non-keratinizing epithelium'. In the vestibulum nasi short hairs (vibrissae) filter large particles from the inhaled air. At the interface between the vestibulum nasi and the cavitas nasi propria, the epithelium changes to the typical ciliated epithelium of the airways. The middle and lower concha are covered by airway epithelium. In the regio olfactoria the upper concha is covered by the olfactory epithelium. In the area of the nasal shells, a rich vascularization is developed, which forms the so-called corpora cavernosa. Thanks to this rich vascular network, the air is heated (mainly in the lower nasal shells).
Paranasal sinuses[edit | edit source]
The secondary nasal cavities in the upper jaw, frontal, olfactory and sphenoid bones are lined with 'thin airway epithelium (mucosa tightly fused to the periosteum), in which there are not as many goblet cells as, for example, in the cavitas nasi. It contains small mucous glands, the secretion of which enters the nasal passages with the help of the movement of the cilia of the epithelium.
Larynx[edit | edit source]
The larynx connects the pharynx and trachea and has a skeleton of hyaline and elastic cartilage. 'The epithelial layer is not the same everywhere. In almost all parts of the larynx, we can find a multi-row cylindrical epithelium with cilia and goblet cells.
Epiglottis[edit | edit source]
The epiglottis is formed by elastic cartilage and is covered by a mucous membrane. Elastic fibers, seromucinous tuboalveolar glands are found in the lamina propria mucosae. It is covered by a double epithelium:
- surface to the tongue: multi-layered squamous epithelium (transitions also to the surface facing the larynx);
- surface to the larynx: in the basal section, the squamous epithelium transitions into the epithelium of the airways;
Right vocal folds (plicae vocales)[edit | edit source]
It is a pair of mucous eyelashes that are supported by an elastic vocal cord (ligamentum vocale). Plicae vocales are covered by multilayered squamous epithelium'' due to greater mechanical stress (faster air flow, mutual contact). The lamina propria does not contain glands, but the so-called Reinke's space, which is filled by a sparse collagenous tissue under the epithelium.
False vocal folds (plicae vestibulares)[edit | edit source]
The plicae vestibulares are covered with airway epithelium (multi-row cylindrical with cilia). The lamina propria mucosae is made of sparse collagenous tissue and is rich in elastic fibers. It contains tuboalveolar seromucinous glands' which secrete secretions to help moisten the surface of the vocal cords, which are glandless. Laryngitis can cause swelling - a danger for small children.
Ventriculus laryngis[edit | edit source]
The space bounded by the lungs (plicae vocales and plicae vestibulares) is lined with airway epithelium. Tuboalveolar glands and islands of lymphatic tissue (tonsila laryngea) are found in the lamina propria mucosae.
Trachea[edit | edit source]
The trachea is a tube 10−12 cm long, which divides into two main bronchi at the point of bifurcation. The mucosa is covered with airway epithelium, except at the bifurcation where we find stratified squamous epithelium. The lamina epithelialis has a thick basement membrane. In the lamina propria we find clusters of lymphocytes, elastic fibers, sparse collagenous tissue, but above all tracheal seromucinous glands - glandulae tracheales.
Under the lamina propria we find a layer called tunica fibromusculocartilaginea. It is formed by regularly arranged hyaline cartilages in the shape of rings which open towards the back. The back wall consists of ligament (paries membranaceus) and circularly arranged smooth muscle (m. trachealis/bronchialis). Individual cartilaginous rings connect the ligg. annularia - fibroelastic membranes.
Links[edit | edit source]
Related articles[edit | edit source]
- Nasal cavity
- Larynx
- Larynx (histological preparation)
- Epiglottis (histological preparation)
- Trachea
- Bronchus (preparation)
- Bronchus segmentalis (histological preparation)
Source[edit | edit source]
References[edit | edit source]
- ↑ Renate Lüllman-Rauch, Histologie, Grada, Praha 2012