Mathematical description of pharmacokinetic processes
Pharmacokinetic methods try to use mathematical relationships to capture the time dependence of the drug's stay in the body. They are based on the analysis of the concentrations of the drug and its metabolites in available body fluids (most often blood , urine and saliva ).
The most important information is:
- about the amount of drug that reached the systemic circulation and the speed with which it did so (bioavailability),
- on the distribution of the drug in the body,
- on the rate of drug elimination.
Mathematical relationships are used to predict drug concentration and individualize dosage . The concentration profile of the drug (dependency of drug concentration on time from administration) is captured in them using basic pharmacokinetic parameters. These are variables that depend on a number of physiological and pathophysiological factors of the organism as well as factors on the side of the drug.
Pharmacokinetic parameters are divided into:
- Primary
Their changes can be directly explained by changes in physiological variables – e.g. blood flow, binding to proteins, glomerular filtration .
- Distribution volume (Vd),
- clearance (CL).
- Secondary
Their size depends on the primary parameters:
- biological elimination half-life (t 1/2 ),
- area under the blood drug concentration curve (AUC),
- bioavailability of the drug (F).
Distribution volume[edit | edit source]
Distribution volume is the ratio between the amount of drug ( M ) in the body and its concentration in the blood (plasma, serum) ( c ):
By rearranging the relationship, we get: amount of drug in the body (M) = V d . c .
It is clear from this form of notation that the distribution volume can also be defined as follows:
The volume of distribution is the volume in which the drug present in the body would have to be homogeneously dispersed (dissolved) in order to achieve the same concentration of the drug as in the blood.
The distribution volume does not represent the real volume. In fact, the drug is distributed unevenly between blood and tissues, mainly depending on its physicochemical properties and binding to blood and tissue proteins. In some cases, Vd can reach very high values. This is the case when the drug binds to a high percentage in the tissues and little to proteins in the plasma . Then its plasma concentration is low and Vd is much higher than the volume of total body water (Vd of quinacrine is 50,000 l).
The unit of distribution volume is the volume unit (liter). However , Vd is often expressed and interpreted in relation to body weight (liter/kg) similarly to, for example, volumes of body fluids (see table).
| Compartment | Volume (l/kg body weight) |
|---|---|
| Plasma | 0.04 |
| Blood | 0.08 |
| Extracellular water | 0.2 |
| Total body water | 0.6 |
| Fat | 0.2–0.35 |
A comparison of the volume of distribution of the drug (vl/kg) and the volumes of total, intracellular, extracellular, and intravascular fluid allows some conclusions to be drawn about the magnitude of distribution. The drug, whose Vd reaches approximately 0.6 l/kg, is distributed from the blood into the extracellular and intracellular space ( methotrexate , erythromycin antibiotic). The drug with Vd = 0.1−0.3 l/kg is distributed into the extracellular space ( gentamicin , vecuronium − like most polar, water-soluble substances). The drug with V d = 0.05 l/kg remains intravascular (heparin). Conversely, a drug whose V d significantly exceeds 0.6 l/kg is distributed intracellularly and additionally binds to cellular structures (lipophilic drugs).
Use of volume of distribution in pharmacokinetic calculations[edit | edit source]
- To calculate the impact (saturation) dose (DN) .
- DN = Vd . cT
- A loading dose is needed to quickly achieve a therapeutically effective blood concentration (cT).
- To estimate the amount of medicine in the body (in case of overdose, in forensic medicine).
- amount of drug = Vd . C
- The concentration in the blood is determined by analysis, and based on the given relationship, the dose of the drug (any substance) is approximately estimated.
- To assess the effect of hemodialysis and hemoperfusion on the pharmacokinetics of the drug. Medicines with a large volume of distribution cannot be effectively removed from the body by these techniques.
Clearance[edit | edit source]
Clearance is the ratio of the rate of elimination of the drug and its concentration in the blood (generally also in another biological fluid, e.g. plasma or serum).
Elimination rate is the amount of drug eliminated per unit time (unit is mol/s, mg/h). The unit of clearance is volume/time (l/h, ml/s, ml/min). Sometimes it is stated in relation to body weight or body surface area (l/h.kg -1 , l/hm -2 ).
Total clearance reflects the overall rate of elimination of the drug from the blood (plasma) and has an additive character, i.e. it includes elimination by all organs (intestines, liver, kidneys, lungs...). Quantitatively, renal and hepatic clearances are usually the most important .
- CL = CLR + (CLJ + next)
Sometimes the term non-renal clearance (the term in parentheses) is used, which is the difference between total and renal clearance.
Renal clearance[edit | edit source]
Renal clearance ( CLR ) is the amount of drug eliminated per unit time by the kidneys, related to the concentration of the substance in the blood ( c ). The amount excreted per unit time is equal to the product of the volume of urine excreted per unit time (volumetric urine flow rate) and the concentration of the drug in the urine ( cU ).
where is the volumetric flow rate of urine (ml/s), cUis the concentration of the drug (generally any substance) in the urine, c is the concentration in the blood. Renal drug clearance is obtained by the same procedure as creatinine clearance. During the collection interval T , a volume of urine V is collected . The average blood drug concentration within the urine collection interval is used in the denominator. If urine is collected long enough (from the time the drug is administered until the drug disappears from the blood), the relationship with AU (total amount of drug excreted in urine) and AUC (area under the curve of blood drug concentration vs. time) is used. Rearranging the relation gives:
Renal clearance can therefore also be understood as the volume of blood (plasma) that is completely cleared of the drug in the kidneys per unit of time.
Similarly, total clearance is the volume of blood (plasma) that is completely cleared of the drug (the volume from which the drug is completely removed) per unit time.
Renal excretion includes the processes of glomerular filtration (GF), active tubular secretion, and active and passive tubular reabsorption. GF and secretion increase renal clearance, while reabsorption decreases renal clearance.
The physiological range for glomerular filtration rate is 80−120 ml/min. In practice, GF is measured using the clearance of an endogenous substance - creatinine ( 'ClKR ). Creatinine does not bind to plasma proteins, it is freely filtered into the primary urine and is not absorbed or secreted in the tubules (active secretion occurs only with pathologically elevated creatinineemia). With normal kidney function, the concentration of creatinine in the blood is relatively constant during the day. This simplifies the calculation:
- GF ≈ Clkr = (cU. V) / (c.T)
where V is the volume of urine, T is the time interval of urine collection, cU and c are the concentrations of creatinine in urine and plasma.
The magnitude of renal clearance allows some consideration of the mechanism of drug excretion. E.g. the renal clearance of ampicillin (283 ml/min) greatly exceeds the amount of glomerular filtration, so we can consider a significant contribution of tubular secretion to the elimination of the drug by the kidneys.
The drug, which is largely excreted unmetabolized in the urine and has a high renal clearance value (≥ 0.1 l/min), accumulates in the body of patients with reduced kidney function. Dosing rate must be reduced (dosing interval extended or even individual dose reduced). There are several ways (tables, nomograms, computer programs) to adjust the dosage of these drugs based on GFR testing.
Hepatic clearance[edit | edit source]
Hepatic clearance (CL J ) is the amount of drug extracted from the blood by the liver per unit of time related to the concentration of the substance in the portal blood:
where Q is the volumetric rate of liver blood flow (1.5 l/min, 90 l/h), cin is the concentration of the drug in the blood entering the organ (in the v. portae) and cout is the concentration in the blood leaving the organ ( in the hepatic vein).
We refer to the fraction as the extraction ratio ( E ). For substances with high hepatic extraction, c out approaches zero and E approaches 1. For substances with very low extraction, c out approaches c inand E is very low (close to zero). The amount of drug clearance when passing through an organ depends on its properties and on the functional state of the eliminating organ. Some drugs are extracted by the liver very efficiently already on the first pass. After oral administration, only a small part of the dose reaches the systemic circulation (< 40%, but for many drugs even less than 10%). We are talking about a significant effect of the first passage of the liver ("first-pass effect"). The elimination of these drugs from the systemic circulation is limited by the speed with which the drug is delivered to the organ (through the blood flow of the liver). The dosage must be reduced in case of impaired liver function, because bioavailability increases after oral administration, which is manifested by higher blood flow limiting organs (e.g. heart failure), including the influence of simultaneously administered drugs, can have a dramatic effect on hepatic (and renal) clearance, and even greater than the disease of the eliminating organ. Blood flow is also affected by age (it is lower in old people).
The relationship between the amount of clearance and the concentration of the drug in the blood (ie, indirectly also the dose) is of fundamental importance for drug dosing.
For most drugs, clearance is constant within the range of concentrations (doses) used in clinical practice. Elimination is not subject to saturation and the rate of elimination is directly proportional to concentration via a proportionality factor, which is clearance:
- elimination rate = Cl. C
This is first-order elimination. The higher the plasma concentration, the greater the amount of drug eliminated per unit time. In graphical terms, the plasma concentration decreases exponentially with time from administration. Pharmacokinetics of the drug is described as linear .
If any of the elimination pathways has a limited capacity and is subject to saturation , the clearance changes depending on the concentration of the drug (it decreases with increasing concentration).
The dependence between the rate of elimination and the concentration of the drug is analogous to enzyme kinetics (the Michaelis-Menten equation). The rate of elimination increases more and more slowly with increasing concentration. Once a certain concentration is reached, the rate of elimination does not increase further (V MAX is reached ). From this concentration, elimination continues at the same rate regardless of the concentration value. In graphical terms, the plasma concentration decreases linearly with time from administration. This is zero-order elimination . It is typical for ethanol , phenytoin for theophylline and acylpyrine after high doses.
Uses clearance in pharmacokinetic calculations[edit | edit source]
- Total clearance determines the steady-state concentration of the drug in the blood during repeated oral administration or continuous infusion of the drug:
- c av ss is the average drug concentration in the interdose interval ( ) at steady state at by repeated dosing D. F is the bioavailability of the drug and t 1/2 is the biological elimination half-life. Proportion the rate of drug delivery into the body.
- where c ss is the steady-state concentration during iv infusion, R is the infusion rate.
- Conversely, total clearance can be used to calculate the maintenance dose or infusion rate needed to maintain a target blood drug concentration at steady state:
- for continuous IV infusion ( R is the infusion rate, e.g. in mg/h).
- for repeated oral administration ( UD is the dose/dosing interval, e.g. in mg/h).
- The numerical value of clearance and the size of its two most important parts (hepatic and renal) indicate the intensity of elimination events in the most important organs and the possible influence of disease in these organs on the pharmacokinetics of the drug and thus on the dosage.
Biological elimination half-life[edit | edit source]
The biological elimination half-life is the time required for the plasma concentration of the drug to decrease to half of the initial value.
- t1/2 = ln 2 / k = 0,693 / k =
where k is the elimination rate constant. It is a secondary pharmacokinetic parameter. Its value is determined by the ratio of two primary parameters (V d and Cl). The unit is the unit of time (hour).
Use of biological elimination half-life in pharmacokinetic calculations[edit | edit source]
- According to t 1/2 and the dosing interval , we can predict the degree of accumulation of the drug in the blood after repeated administration.
- cumulation moderate (the ratio between the concentration after the first dose and at steady state is about 1:2).
- significant accumulation (steady-state concentration is more than twice that after the first dose).
- cumulation low.
- t 1/2 makes it possible to estimate the magnitude of changes (fluctuations) in drug concentration during one dosing interval ( ). For the ratio of the maximum and minimum concentration in the steady state, the relationship applies:
-
- . Extra open brace or missing close brace i.e. small variation within the dosing interval.
-
- . Extra open brace or missing close brace i.e. slight (moderate) variation within the dosing interval.
-
- .Extra open brace or missing close brace i.e. large variation within the dosing interval.
- using t1/2 we estimate the time required to reach a steady state of drug concentrations during its continuous, unchanged administration.
| the number of t 1/2 from the start of drug administration | concentration (in % of steady state concentration) |
|---|---|
| 1 | 50% |
| 2 | 75% |
| 3 | 87.5% |
| 4 | 94% |
| 5 | 97% |
Area Under the Curve – AUC[edit | edit source]
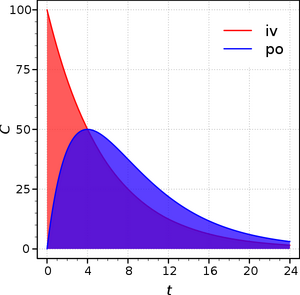
is the area defined by the curve of concentration vs. time, namely:
- in the time interval from the administration of the drug (time 0 h) extrapolated to infinity (for a single administration of the drug),
- in the time interval between two doses (with repeated administration of the drug).AUC - plasma drug concentration as a function of time after iv and after administration
The area under the drug concentration curve (AUC) is the basic quantity in the determination of bioavailability (AUC after single administration, AUC after repeated administration).
Bioavailability (F)[edit | edit source]
is the amount of drug from the dose contained in the administered medicinal product that reaches the systemic blood circulation in a pharmacologically active (in most cases metabolically unchanged) form. It is expressed relatively, i.e. as a part of the dose and can therefore take on values from 0 to 1 (or from 0 to 100 if it is expressed as a percentage). When evaluating bioavailability, the speed with which the active form of the drug reaches the systemic circulation is also important. Thus, bioavailability includes the aspect of quantity (rate of bioavailability) and speed (speed of bioavailability). We distinguish between absolute and relative bioavailability.
Absolute bioavailability[edit | edit source]
Absolute bioavailability is the absolute part of the administered dose that reaches the systemic circulation from the dosage form (after other than intravenous administration). It is determined by comparing the AUC when the drug is administered both in the tested dosage form and intravenously. Absolute bioavailability after intravenous administration is considered equal to 1 (100%), because the drug is applied directly to the systemic circulation and its bioavailability is complete. The loss of the active form of the drug before reaching the systemic circulation is valuable information also from an economic point of view (low absolute bioavailability increases the cost of treatment).
E.g. nisoldipine (calcium antagonist) is completely absorbed, but undergoes metabolism in the intestine and liver. The hepatic first-pass effect is powerful. Ineffective metabolites are excreted by the kidneys. As a consequence, when administered in tablets, its absolute bioavailability is only 5.5%. In patients with liver cirrhosis , the AUC is on average 3 to 5 times higher after administration of the same dose compared to people with a healthy liver. Therefore, it is necessary to administer proportionally lower doses to these patients.
Bioavailability (F) in absolute form is determined by comparing AUC after iv administration (when the entire administered dose reaches the systemic circulation - absorption is 100%) and AUC after extravascular administration, most often oral, when absorption can be affected by a number of events (presystemic elimination , distribution, etc.).
Relative bioavailability[edit | edit source]
Relative bioavailability is the relative fraction of a drug dose that reaches the systemic circulation when comparing the tested dosage form to another dosage form (both are other than for intravenous administration). The rate and speed of bioavailability of the drug from the tested dosage form is therefore compared with its availability from another (reference) dosage form. Relative bioavailability is evaluated in a randomized, crossover study. The drug is administered twice to the same group of healthy volunteers, once in the tested and once in the reference drug form. There is a wash-out period between the two administrations. Pharmacokinetic parameters of the drug are obtained by evaluating the measured concentrations in the blood (plasma, serum) or the amount of the drug excreted in the urine:
- the area under the curve of plasma drug concentrations (AUC), which expresses the degree of bioavailability
- the maximum concentration of the drug in the blood (cmax) and the time needed to reach it (tmax), which express the rate of bioavailability
- in the urine, the total amount of drug excreted in the urine (rate of bioavailability), the maximum rate of urinary excretion and the time to reach the maximum rate of urinary excretion (rate of bioavailability) are evaluated
The bioavailability of a drug is affected by two basic phases: pharmaceutical and pharmacokinetic.
Pharmaceutical phase[edit | edit source]
The pharmaceutical phase decides on pharmaceutical availability, i.e. the amount of drug released from the administered medicinal product that comes into contact with biological membranes and the speed at which this happens. It determines the amount of drug that is available for penetration through the biomembrane. Absorption of the released active drug is preceded by pharmaceutical processes of disintegration, disaggregation and dissolution, which can significantly affect the bioavailability of the drug.
Pharmacokinetic phase[edit | edit source]
The pharmacokinetic phase includes basic pharmacokinetic events: absorption (only for extravascular drug forms), distribution and elimination (biotransformation and excretion).
Clinical significance of bioavailability[edit | edit source]
The clinical significance of drug bioavailability lies in the fact that it allows to assess the relationship between the amount of drug that is administered to the patient and the amount that can actually be used in a pharmacotherapeutic effect. It also informs about the speed with which the drug enters the bloodstream. Since the concentration of the drug in the blood is in a dynamic balance with its effective concentration at the site of action, the data on the bioavailability of the drug in the given dosage form make it possible to derive the onset, intensity and duration of the drug's action. High presystemic elimination (low absolute bioavailability) requires a large difference in the defined content of the drug in the dosage form. This applies especially to oral dosage forms, e.g. beta blockers, nitrates, salicylates, narcotic-type analgesics. The quantitative aspect of bioavailability must be constant so that the physician can rule out an insufficient level of bioavailability as a source of complications in case of unusual or unexpected reactions of the patient to the medicinal product. This requirement also applies to speed. If the relative bioavailability of the drug is equal to 1 (100%), the tested and reference dosage forms are bioequivalent.
By the term biological equivalence (bioequivalence), we refer to the fact that after administration of the same doses of the drug in two dosage forms, there is no greater difference in the rate and speed of bioavailability of the active form of the drug than (most often tolerated) ± 20%. The analytical part of the bioequivalence study (determination of drugs in biological fluids) is governed by the rules of Good Laboratory Practice (GLP). Proof of bioequivalence is important for generics.
Generics are dosage forms containing a known drug whose original versions and dosage forms are no longer protected by the relevant patent. After the patent protection expires, other manufacturers can also take over the production. However, in order for their product (a copy of the original medicinal product, a generic) to be registered, it must be proven that it is bioequivalent to the original product of the manufacturer, who was usually the first to introduce it to the pharmaceutical market. The name "generic" reflects that this medicinal product combines the generic name of the active ingredient with the original product. The importance of the production of generics lies in the fact that their price is significantly lower than the price of the original product, because even the production of generics is cheaper. It does not include the high costs associated with the development of each new entity and its introduction to the pharmaceutical market.
Proof of bioequivalence does not guarantee therapeutic bioequivalence. This must be demonstrated by randomized controlled clinical trials with patients, focused on pharmacodynamic indicators.
Links[edit | edit source]
Source[edit | edit source]
- Ústav farmakologie LF HK UK. . Obecná farmakologie jako základ studia farmakologie experimentální a klinické [online] . 1st edition. Hradec Králové. 2001. 97 pp. Available from <https://www.lfhk.cuni.cz/farmakol/predn/cz/ob/31-60.pdf/>. ISBN 80-902883-4-0.