Leishmania
Leishmania is a genus of parasitic protozoa that causes various forms of the disease, called leishmaniasis . They are among the atypical obligately intracellular flagella (most flagella are extracellular parasites), which invade macrophages in the blood . They are transmitted between vertebrates (eg humans or dogs) by bleeding insects (mainly Phlebotomus and Lutzomia) .
Characteristics[edit | edit source]
Leishmaniasis are IC parasites of phagocytes , all professional, ie. both dendritic cells and neutrophils and especially macrophages (monocytes). The parasite is equipped with properties that allow it to survive in the macrophage by inhibiting oxidative flare (formation of reactive oxygen radicals via the enzyme NADPH-oxidase). They are inhibited by adherence through receptors that serve the macrophage for normal function, or they attach to receptors for complement , and the macrocyte does not find that anything foreign has adhered to it. Thus induced by phagocytosis, the promastygot enters the macrophage in the phagosome, but is unable to block lysosome fusion .with the phagosome, followed by the fusion of the primary lysosomes with the phagosome. Leishmaniasis must be able to develop, multiply and survive the acidic environment of the phagolysosome. They then induce macrophage lysis and are released into the bloodstream. Leishmaniasis are able to infect not only professional phagocytes but also cells that are not, namely fibroblasts, but they do not multiply in them. The presence of leishmaniasis induces changes in fibroblasts that make them "immortal" and risk further releasing leishmaniasis and amplifying the infection.
Life cycle[edit | edit source]
- The life cycle of leishmaniasis consists of two stages. The promasty stage contains a very short flagellum, is infectious to humans and develops in the vector. The second stage is amastygotic and is more important in terms of pathogenicity , it is also whipless and intracellular. The actual transmission is due to bleeding insects, in this case they are very small flies of the genus Phlebotomus.
- The actual transmission is inoculative, the phlebotomus tries to suck blood, but usually it does not succeed the first time due to its small size, so before it finds a suitable capillary, there are several attempts at sucking (probing). Therefore, in some patients, several lesions appear in a row, with each time a probing and a little saliva and infectious promastygotes are inserted into the skin. The vector is small and does not reach too deep, so infectious promastygoths are inserted only into the outer part of the dermis.
- Subsequently, the promastygotes attach to the phagocytic cell and penetrate, transforming into an amastygotic stage. Then they start to multiply inside the phagocyte, the phagocyte is then lysed and the amastytgotes are released.
Occurrence[edit | edit source]
Leismanias are found in 88 countries on five continents, not in Australia and Southeast Asia (it is too humid and hot for carriers). Every year, 2 million people are infected, mostly through the skin, there are about cer viscerals, but they often end in death. It is noteworthy that more than 90% of cases come from six countries - Iraq, Afghanistan, Iran, Saudi Arabia, Syria, Brazil, Peru. Leishmaniasis also occurs in Europe throughout the Mediterranean, from Portugal to Turkey.
Clinical picture[edit | edit source]
Manifestations of the infection are the result of subtle interactions between the innate and acquired human immune response (individual genetic background of the immune response) and the state of the immune system at the time of infection. From the parasite's point of view, there are different types of leishmaniasis that cause different types of diseases. These can be skin or visceral forms, some of which can cause both skin and visceral infections. Virulence and the ability to immunomodulate the responses of an infected host play an important role .
- The resulting clinical manifestation depends on the state of the immune system. The moment the immune system works physiologically, there is a classic skin inflammation , during which inflammatory cells enter the infected site. Cytotoxic reactions occur and infected macrophages are killed. Subsequently, the surrounding tissue is destroyed to eliminate the parasitic nest. The tissue is necrotic and if it heals, it is a very simple form of skin infection. However, if a promastigote that is absorbed by an antigen-presenting phagocyte (eg, dendritic cells) that presents it in the spleen is initially introduced into the skin , the question is whether antigen processing is correct and selection is made for that antigen .specific clone. Depending on the presence of lymphokines in the area, there will be specialization. When pro-inflammatory IL-12 is present in the environment , CD-4 lymphocytes differentiate into TH-1 with the ability to produce interferon γ, which activates macrophages. If the antigen is initially presented to naive CD -4 cells in the presence of anti-inflammatory IL-4 instead of IL-12, another T-cell subclone is selected. These are not able to activate macrophages, ie. that in the presence of IL-12, TH-1 lymphocytes are selected and IFN-γ is produced, which activates macrophages, which produce NO-killing IC leishmaniasis. If IL-4 is present, TH-2 lymphocytes are selected. These do not produce IFN-γ and therefore do not activate macrophages. Leishmaniasis can multiply and the infection spreads.
- There are species of leishmaniasis that cause mainly skin infections ( L. major, tropica, mexicana, braziliensis ), as well as species causing visceral form ( L. infantum, donovani, chagas ). The occurrence of leishmaniasis is limited to the occurrence of carriers. In the old world, phlebotomes of the genus Flebotomus occur and are mainly in the subtropics and semiarid areas (semi-arid). These are the Mediterranean, Iran, Saudi Arabia, India. In contrast, in the New World, especially in Central and South America, there are carriers of Lutzomie, living mainly in very high deciduous areas (Macchu Piccu).
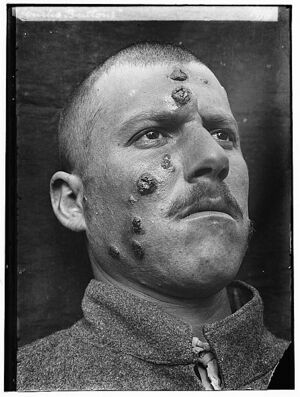
Skin forms[edit | edit source]
- Cutaneous leishmaniasis has 1.5 million cases per year and is divided into localized, recurrent, diffuse. Mucocutaneous can be considered a complication of cutaneous leishmaniasis. The site of the infected macrophages is recognized by the immune system, proliferation occurs, and spontaneous healing ends. The causative agents of the skin form are L. major, L. tropica. The incubation period is 2-8 weeks, sometimes up to three years. At first, a small pimple appears, begins to ulcerate, and forms a central, round ulcer, which gradually grows larger. A round or oval lesion develops that spontaneously heals within a scar within a few months. Recurrent cutaneous leishmaniasis is much rarer. The host repeats the immune response and an uncorrigated hyperallergic reaction occurs, in which only parasites are partially eliminated. Inflammation is activated, an ulcer is formed, which is partially eliminated, but only partially heals, and the infection is reactivated on the circuit - a constantly recurring cycle. They are most common in Iraq. During the diagnosis, it must be taken only from the perimeter of the ulcer, in the center, the leishmaniasis is destroyed. Diffuse cutaneous leishmaniasis is the result of anergy (insufficient or almost no immune response). Stimulation occurscytokines , which suppress the already weakened immune response, and therefore inflammation is virtually non-existent. It is a lifelong infection. There is no spontaneous healing, patients do not respond to treatment. In the old world, only L. ethiopica is evoked . The infection begins with a simple papule on the face, which disseminates and contains a number of parasites. The immune system does not respond to their presence, the lesions never ulcerate, they are very similar to lepromatous leprosy (mycobacterium also infects macrophages). There is a parallel between diffuse cutaneous leishmaniasis and lepromatous leprosy, which no longer occurs in Europe.
Mucocutaneous form[edit | edit source]
- It is unclear etiology, caused by L. braziliensis . It takes place in two phases. The first manifests as a normal localized skin form of leishmaniasis that heals completely. During the second phase, secondary mucosal lesions appear on the nasal mucosa over a period of usually 1-2 months, followed by ulceration of the mucous membranes of the mouth and larynx. Total cartilage destruction can occur. Patients usually die of secondary bacterial infections.
Visceral form[edit | edit source]
- In the latter case, the clinical symptoms are visceral leishmaniasis caused by L. donovani and L. infantum . In the case of visceral leishmaniasis, the infected macrophages are not recognized in the skin, they escape and enter the lymph nodes and then the spleen and bone marrow. The visceral form of leishmaniasis caused by L. infantum (chagasi) occurs in the Mediterranean. From an epidemiological point of view, it is fundamentally different from the kala-azar caused by L. donovani (located only on the Indian subcontinent and in Africa). L. infantum is a zoonosis, the reservoir animal is a dog, a person enters the cycle at random. L. donovaniis anthroponosis, the reservoir is man. After the "cure" of kala-azar, when the internal organs no longer contain lehismania, a certain segment of infected macrophages returns to the skin, where it causes post-kala-azar dermatitis, which is a source for carriers. For this reason, kala-azar is able to create epidemics (eg the Bihar endemic region of India). The incubation period can be weeks to years. Symptoms include high fever and splenomegaly. In the advanced stage, cachectization and muscle atrophy occur. The blood count contains pancytopenia.
Diagnostics[edit | edit source]
The diagnostic procedure involves the determination of specific serum antibodies . For direct identification, the material is puncture from the sternum, the spleen and liver are not punctured because rupture may occur. Peripheral blood, where leishmaniasis cannot be detected, is completely unsuitable for detection.
Therapy[edit | edit source]
Highly toxic pentavalent antimony compounds were originally used for therapy. Liposomal amphotericin is currently used, the liposomal form significantly reducing nephrotoxicity. The zoonic form is important for the Czech Republic. Only 17 cases were recorded in the Czech Republic in the period 1999–2011, most of them imported from Croatia. There is no human vaccination, but since dogs are a common reservoir of infection for phlebotomies, there is a vaccine that protects them from L. infantum .
Links[edit | edit source]
Related articles[edit | edit source]
Reference[edit | edit source]
- TORRES-GUERRERO, Edoardo, Marco Romano QUINTANILLA-CEDILLO and Julieta RUIZ-ESMENJAUD, et al. Leishmaniasis: a review. F1000Res [online] . 2017, vol. 6, p. 750, also available from < https://f1000research.com/articles/6-750/v1 >. ISSN 2046-1402.
References[edit | edit source]
- MILON, Geneva. Perpetuation of Leishmania: some novel insight into elegant developmental programs. Vet Res [online] . 2009 Mar-Apr, vol 40, no. 2, p. 38, also available from < https://www.vetres.org/10.1051/vetres/2009021 ,>. ISSN 0928-4249.
- JÍRA, Jindřich and Ivan VAŘEKA. Medical protozoology: protozoal diseases. 1st edition. Prague: Galén, 2009. 0 pp. ISBN 978-80-7262-381-5 .
- Relapse of kala-azar after use of multiple drugs: A case report and brief review of literature K Pandey, SB Pun, BD Pandey, 28-May-2012, http://www.ijmm.org/article.asp?issn= 0255-0857; year = 2012; volume = 30; issue = 2; spage = 227; epage = 229; aulast = Pandey
- VOKURKA, Martin and Jan HUGO, et al. Great medical dictionary. 5th edition. Prague: Maxdorf, 0000. 1008 pp. Jessenius; ISBN 80-7345-058-5 .