Diseases of the gallbladder and pancreas in children
From WikiLectures
Diseases of the gallbladder and bile ducts[edit | edit source]
- gallbladder anomalies – accompany bile duct atresia or cystic fibrosis
- acute gallbladder hydrops – during generalized infections, sepsis or Kawasaki disease
- manifestations – fever, jaundice, more palpable gallbladder
- treatment – conservative, surgery is indicated only in gangrene of the gallbladder
- cholecystitis – G+ (streptococci) but also G- bacteria (salmonella, shigels), parasites (ascaris, giardia)
- sometimes it is a complication of periarteriitis nodosa and other vasculitis or in Kawasaki disease
- possibly also in Wilson's disease
- therapy - ATB, good hydration
- cholelithiasis – is relatively rare in children
- mainly in obese girls during puberty or after repeated hemolysis (pigment stones) - in our country most often after spherocytosis, in black people after sickle cell disease)
- may also be in CF, Wilson, congenital bile abnormalities. pathways, in IgA deficiency
- clinical picture – nausea, vomiting, jaundice, fever, often colic-like abdominal pain with radiation back and under the right scapula or under the right shoulder
- therapy – surgical, for colic - hydrate well, strict diet and give short-term antispasmodics resp. analgesics (Algifen)
Extrahepatic atresia of the bile ducts[edit | edit source]
- absence of extrahepatic bile ducts
- incidence - 1:14 000 births
- It is thought to be the result of a sclerosing inflammatory process that begins fetally, at delivery or immediately after, etiology unknown
- Newborns are usually born out of a normal pregnancy and are fine immediately after birth
- atresia manifests at the age of several days, max. weeks - cholestatic syndrome , ie prolonged jaundice with a change in the color of urine (dark) and stool (light, acholic)
- percutaneous liver biopsy is important , but there are no typical histological findings that would distinguish it from other liver diseases
- obstruction can be verified isotopically or by ERCP
- surgery - in all infants in whom we have ruled out other liver diseases
- hepatoportoenteroanastomosis is most often used (Kasai's operation) - anastomosis between the hepatic porta and the intestine is established
Diseases of the pancreas[edit | edit source]
- The most common pancreatic disease in children is cystic fibrosis
- otherrs are quite rare
- diagnosis - examination of pancreatic secretion - collection of duodenal juice after secretion stimulation (demanding and burdensome)
- screening test for pancreatic lipase secretion disorder - examination of fat droplets in stool
- PABA test - we administer a peptide from which chymotrypsin cleaves PABA (paraaminobenzoic acid) - it is absorbed and excreted in the urine
Congenital anomalies of the pancreas[edit | edit source]
- annular pancreas
- it is formed by incomplete rotation of the ventral part, the pancreas revolves around the duodenum and jejunum and makes a typical picture of congenital GIT obstruction
- more common in Down syndrome
- symptoms - see stenosis
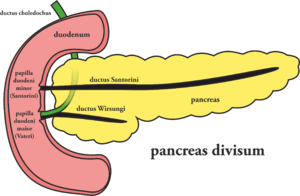
- divided pancreas
- is one of the most common GIT anomalies, mostly it causes only minimal problems or is detected by chance
- the incidence is estimated at 10% of the population
- the result of the disorder is that part of the pancreas (cauda, corpus and part of the head) does not secrete into the ductus Wirsungi, but through the ductus Santorini
- the anterior part may be compressed and chronic pancreatitis may develop
- ectopic pancreatic tissue
- It can be localized in the small intestine or stomach, usually does not cause problems
- sometimes it can cause bleeding, partial obstruction or a intussusception (ie insertion of a part of the intestine into the adjacent part of the intestine)
Congenital disorders of pancreatic excretory function[edit | edit source]
- isolated deficits of pancreatic enzymes - rare
- Johanson–Blizzad syndrome – congenital pancreatic insufficiency, deafness, microcephaly, skull skin defects, hypothyroidism, dwarfism and nasal wing aplasia
- Schwachman-Diamond Syndrome – the most common congenital secretion disorder
- AR, incidence 1:20 000, pancreatic tissue is infiltrated with fat
- clinical picture – malabsorption syndrome, growth and development retardation
- reminds of CF but without finding chlorides in sweat, there are usually more associated congenital diseases
- neutropenia (neutrophils show loss of chemotaxis), metaphyseal dysplasia → growth disorders
- growth disorders persists even with pancreatic replacement. enzymes (unlike CF)
- neutrophilia is cyclical, leads to frequent bacterial infections and often to lethal sepsis
- diagnosis - malabsorption, skeletal changes, disorders of pancreatic secretion, normal Cl concentration in sweat
- on CT is a hypodense pancreas
- therapy - enzyme substitution, consistent and early treatment of bacteria. infections, on neutropenia - G-CSF
- prognosis - severe
Acute pancreatitis[edit | edit source]
- it can accompany or complicate many general childhood diseases
- etiology: infections - parotitis virus, VHA, coxsackie, pancreas is also sensitive to many toxins and drugs
- in adolescents it can occur after alcohol and drugs, in all children after some immunosuppressants or antimicrobial drugs (tetracyclines, sulfonamides ), diuretics, antiepileptics, Au preparations
- occasionally occurs in congenital bile duct and pancreatic disorders, CF, Rey's syndrome and MODS
- from systemic diseases - most often in - CF, DM, binder diffusion disorders, Rey's sy, Kawasaki
- trauma and obstruction of the bile ducts can also be the cause
- pathogenesis: the effect of occlusion of the leads by inflammation, which is caused by a given etiological factor, is presumed, followed by activation of enzymes and escape into the stroma - the most important is the activation of trypsin and chymotrypsin
- autoactivation is controlled by enterokinase, bile regurgitation
- stasis destroys protease inhibitors, which otherwise prevent activation in the pancreas
- necrosis with calcifications and saponification occurs, the process penetrates into the environment
- in a very severe course, there is a risk of circulatory shock and ARDS
- clinical picture: very acute pain
- sudden pain in the epigastrium, the patient locates it in depth, as a fickle, practically permanent pain, radiates to the back (when the cauda is affected, it may radiate to the left shoulder with irritation of the diaphragm)
- vomiting, fever, tachycardia, tachypnoea, sweating and hypothesia prone to collapse
- the pain is extremely intense, the child takes a crouched position, attracts the limbs to the abdomen, usually lies on his side, prevents any change of position and any examination
- the abdomen is hard to the touch, dilated, arched above the level of the chest, sometimes resistance can be felt in the depths of the left epigastrium
- the pain worsens, the peristalsis is weakened or absent
- hypocalcaemia with latent or overt tetany may result from salt deposition
- the most serious form – acute hemorrhagic pancreatitis – is rare in childhood, may be in adolescents after drug or alcohol excess, jaundice, ascites, shock, acute renal insufficiency, DIC, gastrointestinal bleeding, respiratory disorders
- laboratory: vomiting leads to dehydration, hyponatremia, hypochloraemia and potassium depletion, hypocalcaemia is characteristic
- in serum and urine the value of amylases increases within 2–12 hours (decreases in 24–48 hours) - predominance of pancreatic isoenzymes
- increase in serum lipases - with a threefold increase, this value is more specific and sensitive than amylases
- rising ALT , AST , LDH
- leukocytosis and hyperglycemia
- diagnosis: hyperamylasemia is really important
- imaging methods - especially valuable - abdominal sono and CT will provide the most data - pancreatic enlargement, hypoechogenic edematous pancreas, presence of pseudocysts filled with fluid or blood, duct dilatation, sometimes purulent abscesses
- X-ray - non-specific findings - elevation of the left diaphragm arch, small pleural effusion on the left, smaller infiltrates at the base of the lungs or pulmonary atelectasis
- dilated colon transverse, calcification in the pancreas
- ERCP in recurrent pancreatitis
- differential diagnosis: other causes of pain - appendicitis, peptic ulcer, intestinal obstruction, cholecystitis
- other causes of elevated amylases - parotid disease ( mumps , EBV , CMV , HIV , sialoadenitis ), eating disorders (anorexia, bulimia)
- biliary tract diseases, some systemic conditions (burns, head injuries, renal insufficiency, MAc, transplant rejection)
- Acute pancreatitis requires repeated surgical consultation and close cooperation with a pediatric surgeon
- other causes of elevated amylases - parotid disease ( mumps , EBV , CMV , HIV , sialoadenitis ), eating disorders (anorexia, bulimia)
- therapy: no specific therapy
- symptomatic: rehydration, pain relief, pancreatic secretion suppression and complication prevention and treatment
- patients are hospitalized in the ICU and constantly monitored
- pain relief - opiates are contraindicated because they increase the tone of Oddi's sphincter, we use tramadol the most
- we stop the oral supply of anything to the child (this will reduce the secretion)
- we pay attention to rehydration (we monitor CVP), we adjust the internal environment according to acute changes
- we constantly aspirate gastric and duodenal contents with a probe
- the prognosis of acute hemorrhagic pancreatitis still has up to 50% mortality
- serious prognostic indicators - high leukocytosis (above 16.10 9 / l), disproportionate glycemia, high value of LDH and aminotransferases, hypoclacemia below 2 mmol / l, hypoxia and resp. insufficiency
- acute without hemorrhage usually resolves during conservative treatment within 2–4 days, but convalescence is long (0.5–2 years following a strict diet)
Chronic pancreatitis[edit | edit source]
- most often on a genetic basis - such as familial chronic pancreatitis
- etiology: AD, penetration is high (affects all offspring with a defective gene)
- but the expressiveness (degree of disability) is very diverse
- in addition, chronic relapsing pancreatitis can occur in other diseases - inherited hyperlipidemia I., IV. and V., in CF, hyperparathyroidism or as a result of pancreatic anomalies
- clinical picture: at first the symptoms are mild, often just dyspepsia
- they often start at the beginning of school and are related to a change in diet (school canteen)
- takes place in the form of short-term, several-hour seizures
- seizures become more severe
- chronic pancreatic insufficiency gradually develops - it suffers from fat digestion - first steatorrhea, then a picture of malabsorption syndrome
- diagnosis: careful family anamnesis
- during the attack we can detect biochemical changes in pancreatitis
- outside seizures we can detect pancreatic calcification and the development of pseudocysts
- differential diagnosis: we must determine chlorides in sweat, examine serum lipoproteins (exclude hyperlipoproteinemia), Ca and P concentrations, or tests for hyperparathyroidism, we examine the stool for ascaris eggs
- therapy: enzyme substitution, dietary measures (prohibition of alcohol and toxins, adequate protein intake, fat reduction to 35% intake, reduction of simple carbohydrates, fiber preferences (if the pancreas does not fail completely), eat smaller doses more often
Links[edit | edit source]
Source[edit | edit source]
- BENEŠ, Jiří. Studijní materiály [online]. ©2007. [cit. 2009]. <http://www.jirben.wz.cz/>.
References[edit | edit source]
- HRODEK, Otto – VAVŘINEC, Jan. Pediatrie. 1. edition. Galén, 2002. ISBN 80-7262-178-5.
- ŠAŠINKA, Miroslav – ŠAGÁT, Tibor – KOVÁCS, László. Pediatria. 2. edition. Herba, 2007. ISBN 978-80-89171-49-1.