X-linked adrenoleukodystrophy
X-linked adrenoleukodystrophy (also Schilder's disease , sudanophilic leukodystrophy , XALD , X-linked ALD ) is an X-linked recessively inherited disorder of lipid metabolism manifested by neurological symptoms and symptoms of adrenal cortex insufficiency.
Epidemiology[edit | edit source]
XALD is an X-linked recessive disease and therefore primarily affects males, less often heterozygous females. The disease begins to manifest itself at different ages, depending on the clinical form of the disease. It belongs to the most frequently occurring leukodystrophies with a prevalence of 1-5:100,000.
Etiopathogenesis[edit | edit source]
The disease is caused by a defect in the oxidation of very long-chain unbranched fatty acids (C25:0 and C26:0, VLFCA ) due to a deficiency of the peroxisomal enzyme lignoceroyl-CoA ligase . A genetic defect in the ABCD1 (ATP binding cassette, subfamily D, member 1) gene on gonosome X was describedin the Xq28 region. The ABCD1 gene encodes a peroxisomal transmembrane protein that is involved in anchoring lignoceroyl-CoA ligase (VLFCA-CoA synthetase) to the peroxisomal membrane. In this way, VLFCAs, which accumulate, cause cell membrane disruption and are responsible for neurological symptoms, are reduced. Similarly, VLFCAs accumulate in the zona fasciculata and reticularis of the adrenal cortex and cause their dysfunction. VLFCA is abnormally elevated in tissues and tissue fluids.
Clinical forms[edit | edit source]
- children's cerebral
- adolescent cerebral
- adult cerebral
- adrenomyeloneuropathy
- a form manifested only by adrenal insufficiency
- symptomatic heterozygotes
Clinical picture[edit | edit source]
The disease is manifested by neurological symptoms and symptoms of adrenal cortex involvement.
Neurological symptoms include impairment of intellectual functions , behavioral disorders , motor function disorders , and cerebellar ataxia . Sensory disorders gradually develop leading to blindness and deafness . Epileptic seizures may be present .
As a result of hypocorticalism of the adrenal cortex ( Addison's disease ), hyperpigmentation may be present .
The disease has an unfavorable prognosis, it ends fatally within a few years.
Infant cerebral form[edit | edit source]
It is one of the most common forms of XALD. It usually has a more difficult course. The child is without clinical symptoms until the age of 4 to 10 years, behavioral disorders and failure to thrive in school will begin to appear as the first symptom. There is a regression of auditory discrimination, orientation in space, speech and writing. Typically, the clinical condition rapidly progresses to spastic paraparesis, difficulty swallowing, loss of vision, and within two years of the first symptoms to a vegetative state .
Adolescent cerebral form[edit | edit source]
The disease manifests itself between the ages of 10 and 21. It is rare. Clinical symptoms are similar to the pediatric form, but the progression is slower.
Adult cerebral form[edit | edit source]
It manifests after the age of 21 with symptoms such as dementia, spastic paraparesis and psychiatric problems. It is relatively rare, accounting for about 3% of all XALD cases. The disease has a rapid course and progresses to a vegetative state after about 3-4 years.
Adrenomyeloneuropathy[edit | edit source]
It is the most common form of XALD, accounting for 40% of cases of this disease. Adrenomyeloneuropathy is characterized by progressive myelopathy leading to spastic paraparesis. Until 5-15 years, the patient is confined to a wheelchair. The first symptoms usually appear between the ages of 20 and 30 and include stiffness and clumsiness of the legs, weight loss, nausea and generalized weakness. Sphincter disorders and impotence are also present. Other symptoms may be of cerebellar origin, intellectual deterioration and behavioral disorders. Adrenal dysfunction may not be accompanied by hyperpigmentation, stress tests can demonstrate insufficiency. An increased concentration of long-chain fatty acids is diagnostically conclusive. The disease leads to invalidation, but does not shorten the life span.
Symptomatic heterozygotes[edit | edit source]
Most heterozygous women do not manifest the disease, however, some heterozygotes may develop XALD. The symptoms can be different, ranging from mild to severe, but the adrenal glands are very rarely affected.
Diagnostics[edit | edit source]
The increased amount of fatty acids with a very long chain in serum and skin fibroblasts is evident.
A blood DNA test will prove the presence of the mutation.
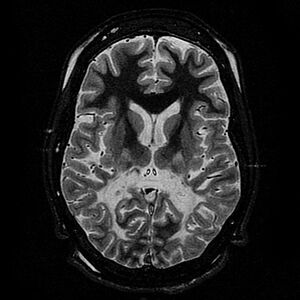
Imaging methods such as CT and MRI will demonstrate extensive demyelinating changes in the brain that begin occipitally and gradually spread in a frontal direction.
In the cerebrospinal fluid, there is usually protein cytological dissociation , sometimes pleocytosis . An increased level of intrathecal IgG is usually a sign of rapid progression.
Therapy[edit | edit source]
There is no effective treatment.
Dietary precautions are controversial in XALD. There are studies that try to prove the effectiveness of the so-called "Lorenzo oil" , a mixture of glycerol trioleate and glycerol trierugate in a ratio of 4:1. Lorenzo's oil normalizes long-chain fatty acid levels within 4 weeks and may reduce the frequency and severity of neurological symptoms if administered before symptoms appear.
Bone marrow transplantation has a limited effect and is indicated only in the preclinical stages of the disease.
Hormonal replacement is given for manifestations of insufficiency of the adrenal cortex.
XALD therapy options are the subject of research.
Links[edit | edit source]
Related Articles[edit | edit source]
- Peroxisomal leukodystrophy
- Leukodystrophy
External links[edit | edit source]
- United Leukodystrophy Foundation, Inc.
- Lorenzo's Oil movie
References[edit | edit source]
- UNITED LEUKODYSTROPHY FOUNDATION, INC,. www.ulf.org [online]. [cit. 2011-12-02]. <https://ulf.org/types/XALD.html>.
- ↑ Skočit nahoru k:a b c d e f g h i j k l m n o p NEVŠÍMALOVÁ, Soňa, Evžen RŮŽIČKA a Jiří TICHÝ. Neurologie. 1. vydání. Praha : Galén, 0000. 0 s. ISBN 80-7262-160-2.
- ↑ Skočit nahoru k:a b c d e f g GOETZ, Christopher G a Christopher G GOETZ. Textbook of clinical neurology. 3. vydání. Philadelphia : Saunders Elsevier, 0000. 0 s. ISBN 1-4160-3618-0.
- ↑ MOHNISH, Suri. Genetics for pediatricians [online]. [cit. 2011-12-02]. <https://books.google.cz/books?id=tBSi9heXrG4C&pg=PP7&lpg=PP7&dq=Genetics+for+pediatricians+isbn&source=bl&ots=gxLZmZBSHM&sig=TUutKIU8m9b9o02M9Vi45PvpC4A&hl=cs&ei=ZvPYTv6jA8Xa4QTK4OSGDg&sa=X&oi=book_result&ct=result>.
| Hereditary Metabolic Disorders (HMDs) | |
|---|---|
| In general | DMP of complex molecules • DMP of small molecules • Newborn screening • Screening for hereditary diseases • Examination methods for DMP |
| DMP amino acids | Alkaptonuria |
| Organic aciduria | – |
| DMP of the urea cycle | Alkaptonuria • Ornithine transcarbamylase deficiency • Prolidase deficiency • Phenylketonuria • Glutaric aciduria • Hyperphenylalaninemia • Hyperornithineemia • Isovaleric aciduria • Leucinosis • Nonketotic hyperglycinemia • Cystinosis • Tyrosinemia |
| DMP of propionate, biotin
and cobalamin |
Biotinidase deficiency • Methylmalonic acidemia • Propionic acidemia |
| DMP of purines and pyrimidines | Hepatic porphyria • Cutaneous porphyria • Mitochondrial neurogastrointestinal encephalomyopathy |
| DMP sugars | Glycogenoses • Fructoaldolase deficiency • Fructose-1,6-bisphofatase deficiency • Essential fructosuria • Galactokinase deficiency • Galactose-1-phosphate uridyltransferase deficiency |
| Mitochondrial DMP | Phosphoenolcarboxykinase deficiency • LCHAD deficiency • MCAD deficiency • Pyruvate dehydrogenase deficiency • Pyruvate carboxylase deficiency • SCAD deficiency • Chronic progressive external ophthalmoplegia • Leber's hereditary optic neuropathy • Leigh syndrome • Maternal diabetes and deafness • Kearns-Sayre syndrome • VLCAD deficiency |
| DMP of peroxisomes | Neonatal adenodystrophy • Refsum disease • Rhizomelic chondrodystrophia punctata • X-linked adrenoleukodystrophy • Zellweger syndrome |
| DMP of lysosomes | Fabry disease • Gaucher disease • Krabbe disease • Danon disease • Mucolipidosis II • Metachromatic leukodystrophy • Mucopolysaccharidosis III • Niemann-Pick disease • Cystinosis • Tay-Sachs disease |
| Portal: Pathobiochemistry | |