Thymus
Thymus - structure, position and syntopy, function
Introduction[edit | edit source]
- Primary lymphoid organs are where lymphocytes first originate, including the thymus and bone marrow, while secondary lymphoid organs are where most lymphocyte get activated and proliferate for eg: in lymph nodes, spleen, tonsils, MALT , GALT etc.
- The thymus is fully functional at birth, remaining active until puberty when it gradually declines in size, cellularity, and T cell production - the size of the thymus decreases with age (it is replaced by adipose tissue)
Anatomical structure and position[edit | edit source]
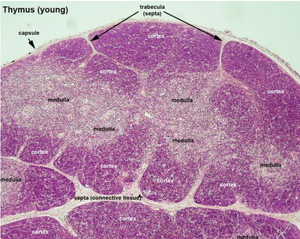
Anatomically, the thymus is an asymmetric, flat organ primarily located in the superior mediastinum, situated posterior to the manubrium of the sternum. Encased in a connective tissue sheath, it forms incomplete lobules consisting of cortical and medullary components.
- The cortical portion, found peripherally within each follicle, contains lymphocytes supported by reticular epithelial cells
- The medullary portion (found centrally) houses fewer lymphocytes and more reticular epithelial cells, including Hassall's corpuscles.
The function of the thymus[edit | edit source]
Functionally, the thymus serves as the site for T-lymphocyte differentiation and the elimination of T cells reactive against self-antigens through a process known as thymic selection. Epithelial reticular cells produce paracrine factors crucial for T-lymphocyte development, selection, and migration.
T cell maturation and selection[edit | edit source]
Initially, lymphoblasts arriving from the bone marrow lack expression of CD4, CD8, or a TCR. They populate the cortex, undergo proliferation, recombine TCR genes, and eventually express CD4, CD8, and TCRs.
This process involves a two-stage selection mechanism:
2 step selection in thymus
- 1st step: Positive selection, occurs in the cortex of the thymus. Here, developing T cells (thymocytes) are exposed to self-antigens presented by thymic epithelial cells (TECs) on major histocompatibility complex (MHC) molecules. T cells expressing T cell receptors (TCRs) that can weakly bind to self-antigens presented on MHC molecules receive survival signals and progress to the next stage of development. Those T cells unable to recognize self-antigens undergo apoptosis (cell death) and are removed from the pool of developing T cells.
- 2nd step: Negative selection, takes place in the medulla of the thymus. Medullary thymic epithelial cells (mTECs) and dendritic cells present a wide range of self-antigens to the developing T cells. T cells with TCRs that strongly bind to self-antigens are eliminated through apoptosis to prevent the development of potentially harmful auto-reactive T cells. T cells that survive negative selection and pass this stage are released into the bloodstream as mature, self-tolerant T cells ready to perform their functions in the immune system.
Vasculature[edit | edit source]
Regarding its vasculature,
- arterial supply: anterior intercostal arteries & small branches from the superior thyroid, inferior thyroid and internal thoracic arteries
- venous drainage: into left brachiocephalic vein and the right internal thoracic vein
References[edit | edit source]
- JUNQUEIRA, L.Carlos – CARNEIRO, Thing, et al. Fundamentals of Histology. 7. edition. Jinocancy. 1999. ISBN 8085787377.