Thoracic aortic dissection
From WikiLectures
- Thoracic aortic dissection is a sudden vascular event with a dramatic course, immediately life-threatening.
Pathogenesis[edit | edit source]
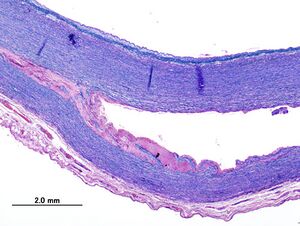
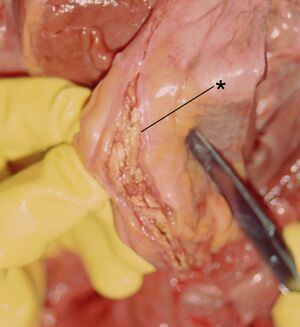
- The cleavage of the aortic wall caused by the penetration of blood through the crack in the intimate and media.
- The rupture occurs most often above the coronary arteries or in the aortic isthmus.
- From the site of the crack, the dissection can spread peripherally and centrally, it can affect the whole circumference or only a part. The canal can also spread to the carotid or visceral branches of the aorta.
- At the end of the dissection, another reentry may occur and a communicating channel is created.
- Consequences
- The canal oppresses the right aortic lumen even at intervals.
- The dissection created above the coronary arteries often spreads centrally and tears the commissures of the aortic valve, resulting in severe insufficiency.
- Causes
- Degenerative media changes ( cystic medionecrosis ) or aneurysm in combination with hypertension , less often atherosclerosis .
- We often encounter it in Marfan's syndrome (young patients) and in other systemic connective tissue diseases ( Ehlers-Danlos syndrome , Loyes-Dietz syndrome ).
- Other predisposing factors include bicuspid aortic valve , aortic coarctation or trauma (falls, car accidents).
CLICK ON LINK FOR VIDEO ON AORTIC DISSECTION:
https://www.wikiskripta.eu/w/Soubor:Aortic_dissection.webm#file
Classification[edit | edit source]
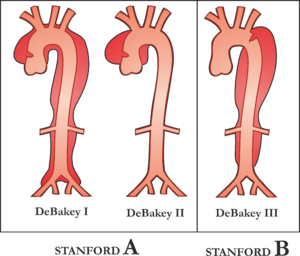
DeBakey classification[edit | edit source]
- Type I - begins in the ascending aorta and continues to the abdominal,
- Type II - bounded on the area of the ascending aorta,
- Type III - begins in the aortic isthmus and affects the descending aorta, or. continues to the abdomen.
Stanford classification[edit | edit source]
- Type A - the ascending aorta is affected (2x more common than type B),
- Type B - affected is the descending aorta.
Clinical picture[edit | edit source]
- Sudden shocking pain behind the sternum and back can progress to the abdomen.
- Sometimes a shock condition follows ( bleeding , tamponade , acute heart failure) - they usually die of sudden death.
- Sometimes the symptoms gradually subside and the condition stabilizes temporarily or permanently.
- Vascular symptoms:
- different, depending on which aortic branches are oppressed or torn off,
- cranial arteries - unconsciousness, hemiparesis,
- subclavia - ischemia HK,
- upper mesenterics - intestinal ischemia,
- renal arteries - anuria , oliguria ,
- peripheral arteries - deficit or asymmetry of pulsations (typically variable over time), lateral asymmetry of pressures on HKK, etc.
Diagnosis[edit | edit source]
- Typical history (sudden acute pain),
- physical examination: deficiency or asymmetry of pulsations in peripheral arteries,
- auxiliary methods:
- exclusion of AIM ( ECG ),
- Chest X-ray - extension of the shadow of the upper mediastinum to the left,
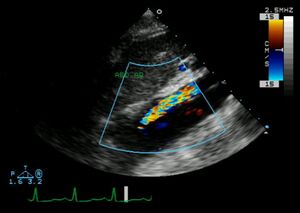
- ECHO , CTA , aortography.
- The sovereign method - transesophageal echocardiography - determines the diagnosis in 98%.
Indications for operation[edit | edit source]
- By type, extent, vascular disability and general condition:
- for type A, about half of the victims die within 24 hours, the hope decreases with each passing hour → type A is always indicated for immediate surgical treatment,
- for type B, we choose a predominantly conservative procedure if there is no vascular symptomatology or there is no risk of rupture.
Therapy[edit | edit source]
- Immediately after the diagnosis, we start drug treatment: antihypertensives , beta blockers and vasodilators , diuresis support . We monitor the patient, administer analgesics (insufficient pain treatment leads to antihypertensive failure). Cardiac tamponade should be ruled out by echocardiography in patients with hypotension.
Type A[edit | edit source]
Principle of operation - we try to cancel the inflow into the aneurysm, several methods:
- transverse intersection of the ascending aorta at the site of the rupture, suturing of both ends of the aorta over the outer and inner meshes, subsequent suture of the aorta,
- resection of the ascending aorta, strengthening of the ends with a suture and replacement of the aorta with a prosthesis,
- Bental's operation - replacement of the aortic valve and ascending aorta by a conduit with a valve, implantation of coronary arteries into the prosthesis,
- closing the entrance to the dissection with tissue glue with aortic suture or with a prosthesis,
- implantation of an intraluminal ring prosthesis into the ascending aorta.
Type B[edit | edit source]
- We treat uncomplicated type B dissection conservatively (stabilization, antihypertensives).
- For complicated dissections, it is necessary to proceed to invasive treatment:
- endovascular stent graft implantation,
- surgical solution.
Principle of surgical treatment
- In the right flank, from a left thoracotomy, usually without ECC, a bypass is sometimes used to protect the kidneys and spinal cord from ischemia .
- Resection of a section with a crack, replacement with a prosthesis, or implantation of an intraluminal prosthesis - this will cancel the entry and it will close with thrombosis. The operation is more complicated when the visceral arteries leave the dissection canal - a laparotomy must be performed and those arteries reconnected to the aorta.
Complication[edit | edit source]
Stanford A dissection can cause acute aortic insufficiency, heart failure, hypotension. Closure of the coronary arteries by dissection leads to AIM (most often a diaphragmatic infarction occurs by occlusion of the ACD ). Rupture of the pericardial dissection creates a cardiac tamponade.
Stanford B dissection can be complicated by spinal, visceral, renal or limb ischemia.
Links[edit | edit source]
[edit | edit source]
External links[edit | edit source]
- Aortic dissection - video on youtube.com NEFČNÍ
References[edit | edit source]
- ZEMAN, Miroslav, et al. Special surgery. 2nd edition. Prague: Galén, 2006. 575 pp. ISBN 80-7262-260-9 .
- ČEŠKA, Richard, ŠTULC, Tomáš, Vladimír TESAŘ and Milan LUKÁŠ, et al. Internal. 3rd edition. Prague: Stanislav Juhaňák - Triton, 2020. 964 pp. ISBN 978-80-7553-780-5 .
Source[edit | edit source]
- BENEŠ, Jiří. Study materials [online]. [feeling. 5/17/2010]. < http://jirben.wz.cz >.