Tetanus
Tetanus is a disease caused by a bacterial neurotoxin Clostridium tetanus , manifested by tonic-clonic convulsions skeletal muscle.
Etiopathogenesis[edit | edit source]
The disease is caused by anaerobic exotoxin, Gram-positive bacteria, Clostridium tetani, rods commonly found in the soil and intestines of mammals, especially horses. Clostridium tetani forms endospores characterized by almost zero metabolism and extreme resistance (especially to heat and radiation). Under certain circumstances (e.g., elevated temperature, low pH, and the presence of water), the endosporus changes to a metabolically active exotoxin-forming form by germination.[1]
Tetanotoxin is an exotoxin of the bacterium Cl. tetani, which consists of three components - neurotoxic tetanospasmin, hemolytic tetanolysin and an enzyme with renin effects. Tetanospasm is responsible for the characteristic clinical picture of tonic-clonic seizures.[1]
Intoxication in humans occurs either exogenously, for example in contact with contaminated soil with a broken skin cover, or endogenously, where the source of infection is intestinal spores, or. vagina. After intoxication, the toxin spreads through the blood and lymph to the neuromuscular discs and from there through the nerve bundles (axons[2]) further into the CNS to motor neurons. The incubation period is usually one week (due to the resistance of the spores, the incubation period can be much longer [3]). Membrane penetration of tetanospasmin is similar to that of botulinum toxin, with the first fragment of the toxin forming a pore in the membrane and the second fragment penetrating the cell. The toxin inhibits the release of the inhibitory neurotransmitters glycine and GABA, lowers the threshold for motoneuron excitability, and develops an image of tonic-clonic seizures.[1] At high concentrations, tetanus toxin can act as a botulinum toxin, thus inhibiting the release of acetylcholine at cholinergic synapses.[2]
If the disease lasts for more than 5 days, demyelination and gliosis occur in the nervous tissue, and in severe cases also hemorrhage.[2]
Clinical picture[edit | edit source]
Before developing the characteristic clinical picture, prodromes appear: feelings of muscle strain, insomnia, sweating and restlessness.[3]
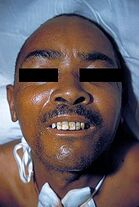
The cramps first affect the facial muscles, which manifest as risus sardonicus (spasmodic smile) and trismus (jaw contracture). The muscles of the back are also affected, when the body bends backwards in an arc, the so-called opistotonus.[1]. The irritation threshold decreases, the patient is hypersensitive, has hyperreflexia. Head tetanus is complicated by laryngospasm and tends to be malignant.[3] The patient is stressed by anxiety, mental and physical agony while fully conscious.
Mortality is high. Death usually occurs between 3-5. the day after the onset of symptoms due to asphyxia from respiratory muscle spasm or due to heart failure with increased afterload.[2]
Differential diagnosis[edit | edit source]
- Stiff-person syndrom –trismus is not typical for this syndrome[2]
- Moersch-Woltman syndrome[2]
Diagnostics[edit | edit source]
Tetanus can be diagnosed according to a characteristic clinical picture.[3]
Atypical forms can be diagnosed by serological detection of antibodies.[3]
To confirm the diagnosis, an excision or scraping of the base from the suspected wound is sent to the microbiologist. Cl. tetani is positive in Gram stain, but it is better to stain with the immunofluorescent conjugate and cultivate further. The presence of tetanospasmin is demonstrated by a neutralization experiment in mice.[1]
Therapy and prognosis[edit | edit source]
Therapy consists of surgical treatment of the wound, administration of anti-tetanus human immunoglobulin IgG (TEGA) (in developed tetanus[1] or preventively in the unvaccinated[4]) resp. revaccination anatoxinem (toxoidem), ATB therapy (ampicillin i.v.), muscle relaxation and respiratory support.[3]
The patient should be surrounded by a quiet environment with a minimum of distractions.[2]
Despite specific therapy, mortality is still high (50% lethality)[3]).In general, the shorter the incubation period, the worse the prognosis. Head tetanus has a worse prognosis, and local tetanus on the limbs has a better prognosis, which can also heal spontaneously. The incidence in our country is sporadic, but over a million people die of this disease every year. [3]
| AGE | CRITERION | ANATOXIN (dose) | TEGA |
|---|---|---|---|
| <15 years | × | × | |
| imunodeficit | ✔ | ✔ | |
| > 60 years | vaccination in the last 10 years | × | × |
| vaccination> 10 years ago | ✔ | × | |
| incompletely vaccinated | ✔ | × | |
| unvaccinated | ✔ | ✔ | |
| > 60 years | ✔ | ✔ |
![]() In unvaccinated individuals, the first dose of toxoid is followed by two more doses at monthly intervals.
In unvaccinated individuals, the first dose of toxoid is followed by two more doses at monthly intervals.
Immunity and prevention[edit | edit source]
The past disease does not leave immunity, the toxin is quickly taken up by nervous tissue and thus there is insufficient contact with immunocompetent cells.[1]https://www.wikiskripta.eu/w/Speci%C3%A1ln%C3%AD:Zdroje_knih/8023802976
Prevention consists in active immunization with tetanus toxoid, a substance without toxic properties but with preserved immunogenicity. Sufficient antitoxin levels in the blood to prevent tetanus are 0.01 UA (antitoxic units)https://www.wikiskripta.eu/w/Tetanus#cite_note-Bed-5. In addition to toxoid, hyperimmune human immunoglobulin IgG is used for prophylaxis in regularly unvaccinated individuals. Specific values can be found in lecture by Dr. Aries.[4]
![]() From January 2018, there is a change in the hexavaccine scheme from 3 + 1 to 2 + 1. The first dose is given from 9 weeks of age, the second 2 months after the first, that is, approximately 4 months, and the third, revaccination, between 11 and 13 months of age. The 3 + 1 scheme applies to premature vaccinations
From January 2018, there is a change in the hexavaccine scheme from 3 + 1 to 2 + 1. The first dose is given from 9 weeks of age, the second 2 months after the first, that is, approximately 4 months, and the third, revaccination, between 11 and 13 months of age. The 3 + 1 scheme applies to premature vaccinations
Until 2018, they were vaccinated against tetanus as part of the https://www.wikiskripta.eu/w/O%C4%8Dkovac%C3%AD_kalend%C3%A1%C5%99
Tetanus toxoid is part of the https://www.wikiskripta.eu/w/Hexavakc%C3%ADna which is given in four doses. The 1st dose is given after the completed 9th week (after the old until 2018 it was until the 13th week after birth), the 2nd dose 2 months after the 1st dose (after the old 1 months after the 1st dose), (after the old 3 dose 1 month after the 2nd dose and 4th dose 6 months after the 3rd dose, but no later than 18 months of age). From Revaccination follows at 5-6 years of age and at age 15 , then revaccinated regularly every 10-15 years https://www.wikiskripta.eu/w/Tetanus#cite_note-Ber-8
Links[edit | edit source]
[edit | edit source]
External links[edit | edit source]
Reference[edit | edit source]
- https://www.wikiskripta.eu/w/Tetanus#cite_ref-bene.C5.A1_1-0 , https://www.wikiskripta.eu/w/Tetanus#cite_ref-bene.C5.A1_1-1 BENEŠ, Jiří, et al. Infectious medicine. 1st edition. Galén, 2009. 651 pp. 275, 276. https://www.wikiskripta.eu/w/Speci%C3%A1ln%C3%AD:Zdroje_knih/978-80-7262-644-1
- https://www.wikiskripta.eu/w/Tetanus#cite_ref-2 WHO. Tetanus (total) reported cases [online]. World Health Organization, © 2015. Last revision 2015-09, [cited. 2018-04-19]. < http://apps.who.int/immunization_monitoring/globalsummary/timeseries/tsincidencettetanus.html
- https://www.wikiskripta.eu/w/Tetanus#cite_ref-3 ZARA, Pavel. Tetanus is a dangerous disease [online]. [feeling. 08-12-2019]. < https://www.fnbrno.cz/tetanus-je-nebezpecne-onemocneni/t6643
- https://www.wikiskripta.eu/w/Tetanus#cite_ref-4 MUDr. Vladimír Motyčka, CSc., Surgical Society, Czech Medical Society of Jan Evangelista Purkyně, < http://www.cls.cz/dokumenty2/resitele/t188.rtf
- https://www.wikiskripta.eu/w/Tetanus#cite_ref-Bed_5-0 https://www.wikiskripta.eu/w/Tetanus#cite_ref-Bed_5-1 https://www.wikiskripta.eu/w/Tetanus#cite_ref-Bed_5-2 https://www.wikiskripta.eu/w/Tetanus#cite_ref-Bed_5-3 https://www.wikiskripta.eu/w/Tetanus#cite_ref-Bed_5-4 https://www.wikiskripta.eu/w/Tetanus#cite_ref-Bed_5-5 https://www.wikiskripta.eu/w/Tetanus#cite_ref-Bed_5-6https://www.wikiskripta.eu/w/Tetanus#cite_ref-Bed_5-7https://www.wikiskripta.eu/w/Tetanus#cite_ref-Bed_5-8https://www.wikiskripta.eu/w/Tetanus#cite_ref-Bed_5-9 BEDNÁŘ, Marek, Andrej SOUČEK and Věra FRAŇKOVÁ, et al. Medical microbiology: Bacteriology, virology, parasitology. 1st edition. Prague: Marvil, 1996. 558 pp. https://www.wikiskripta.eu/w/Speci%C3%A1ln%C3%AD:Zdroje_knih/8023802976
- GOETZ, Christopher G and Christopher G GOETZ. Textbook of clinical neurology. 3rd edition. Philadelphia: Saunders Elsevier, 0000. 0 pp. https://www.wikiskripta.eu/w/Speci%C3%A1ln%C3%AD:Zdroje_knih/1-4160-3618-0
- NEVŠÍMALOVÁ, Soňa, Evžen RŮŽIČKA and Jiří TICHÝ. Neurology. 1st edition. Prague: Galén, 0000. 0 pp. https://www.wikiskripta.eu/w/Speci%C3%A1ln%C3%AD:Zdroje_knih/80-7262-160-2
- BERAN, Ondřej. Vaccination [online]. Last revision 2008, [cited. 2011-12-29]. < http://www1.lf1.cuni.cz/~hrozs/ockovaniOB/OckovaniOB.pdf , http://www1.lf1.cuni.cz/~hrozs/ockovaniOB/OckovaniOB.pdf
- Scattered, Hanuš. . Basics of infectious medicine. - edition. Charles University in Prague, Karolinum Press, 2015. 572 pp. 312. https://www.wikiskripta.eu/w/Speci%C3%A1ln%C3%AD:Zdroje_knih/8024629321