Testicular descent
During embryonic development, the testicles are first located in the abdominal cavity. After a certain time, no later than 3 months of age, the testicles descend from the abdominal cavity through the inguinal canal to the scrotum. If both testicles do not descend, it results in the infertility of the individual.
Embryology and postnatal development[edit | edit source]
The testicles (testes) develop in the retroperitoneum in the prenatal period. Only over time do they descend into the scrotum . Around week 12, the testicles normally reach the inguinal canal, pass through the canal around week 28, and descend into the scrotum around week 33.
In newborns, the testicles are located in the scrotum in 97% of cases (in premature babies, they are more often undescended). In the majority of remaining boys, the descent will, in most cases, complete spontaneously within the first three months of life.
At the end of the second month, the testis with the rest of the mesonephros is attached to the posterior wall of the abdominal cavity by the plica urogenitalis. Caudally, this bar passes into the fibrous band of the gubernaculum testis. Before the testicle descends, it ends at the lower edge of the differentiating external and internal oblique abdominal muscles. Later, when the testicle begins to descend, the extra-abdominal section of the gubernaculum differentiates, growing from the inguinal region into the scrotal mound. As the testicle passes through the inguinal canal, this section of the gubernaculum is fixed to the base of the scrotum. In the female sex, the gubernaculum is also formed and persists as a round ligament of the uterus. ovary proprium.
Factors that influence the descent of the testicle are gradually being discovered. It is clear that the intra-abdominal phase of descent is influenced by the signaling molecule INSL-3, which is produced by the Leydig cells of the testis. The transinguinal phase of descent is apparently under the influence of testosterone .
Disorders of testicular descent (cryptorchism)[edit | edit source]
If one or both testicles do not descend, we speak of Cryptorchidism. It is the most common congenital genital defect in boys. Long-term, abnormal placement of the testicle can lead to reduced fertility in adulthood, and such a testicle is also at increased risk of developing a malignant tumor. Therefore, in indicated cases, it is necessary to start adequate treatment, which is hormonal and/or surgical.
Classification of positional anomalies[edit | edit source]
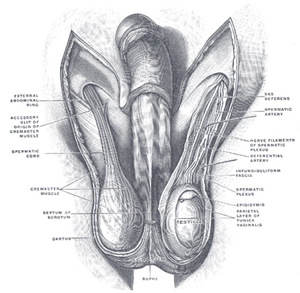
Retractable testicles cannot be considered true cryptorchidism. This is an occasional migration of the testicle due to increased activity of the cremasteric reflex. With gentle manipulation, the testicles can be pulled back into the scrotum. As long as the activity of the muscle fibers of the cremaster muscle is limited, e.g. in Turkish sitting or in a warm bath, it remains in place. Retinal testis = true cryptorchidism is a case where the testis is located somewhere along the path of physiological descent. It can be placed abdominally, inguinally or suprascrotally. We refer to a condition where the retained testicle can be retracted into the scrotum as a sliding testicle , but it returns to its non-physiological position immediately after the pull is allowed. Ectopic testicles describes a condition in which the testicle is placed completely outside the area of physiological descent. In the largest number of cases, it is found laterocranially from the external inguinal ring, but sometimes it can also be found on the perineum, at the root of the penis or in the bilateral half of the scrotum. Testicular agenesis (anorchy) means that the testicle is not developed at all. The spermatic vessels end blindly, the vas deferens can be variously developed. Anorchy is most often the result of torsion or other disruption of the vascular supply, which arose after the 3rd month of intrauterine development.
Examination and treatment[edit | edit source]
A calm environment and patience on the part of both the examinee and the examiner are necessary for the correct examination of the position of the testicle. Immediately after exposing the scrotum, we perform an aspect that precedes the examination by palpation. If a child is examined, the presence of one parent is always necessary. It is important during palpation to have sufficiently warm hands and to be careful not to trigger the cremasteric reflex unnecessarily. We examine the patient standing, in Turkish sitting and lying down. In the Turkish sitting position, the greatest relaxation of the abdominal muscles occurs, thereby limiting the effect of the cremaster muscle contraction. If the testicle is not palpable, it is also necessary to examine the places of possible ectopic placement. Adequate treatment should be started immediately after the 10th month of age and should be completed by the 24th month of life at the latest. It is possible to use conservative and surgical treatment. Conservative treatment includes hormonal treatment, which we can only use in cases where no mechanical obstruction is proven and with high retention. We use surgical treatment if it is not possible to use hormonal treatment, or if this treatment has not been successful.
Links[edit | edit source]
[edit | edit source]
References[edit | edit source]
- ŠMAKAL, Ondřej. Polohové anomálie varlat. Pediatrie pro praxi [online]. 2002, y. 2002, vol. 2, p. 64-66, Available from <http://www.pediatriepropraxi.cz/pdfs/ped/2002/02/05.pdf>. ISSN 1803-5264.
- ADLER, Thomas W. Langmanova lékařská embryologie. 1. vydání. Praha : Grada, 2011. 432 s. ISBN 978-80-247-2640-3.
Kategorie:Pediatrie Kategorie:Embryologie Kategorie:Urologie Kategorie:Anatomie