Radioactivity Practical (Group 1)
|
Check of this article is requested. Suggested reviewer: Carmeljcaruana |
Introduction[edit | edit source]
Radioactivity is a physical phenomenon discovered in the late 19th century by Henri Becquerel. During this physical process a nucleus of an unstable atom loses energy by shedding some of its particles, or excess energy, in the form of γ rays
Radioactive decay can proceed in 3 ways. Either by emitting α, β or γ particles. An α particle resembles nucleus of helium, therefore having 2 protons and 2 neutrons. There are 2 subtypes of β decay; β- and β+. β- decay occurs when a neutron transmutes into a proton, which releases an electron and an electron antineutrino. Whereas β+ decay occurs when a proton transmutes into a neutron, which releases a positron and an electron neutrino. β+ decay can also be called positron emission. Lastly, γ decay is a form of dissipation of excess energy by using photons. All the above mentioned processes are completely spontaneous
Fig. 1.1 - Examples of α,β, γ radiation
Clinical importance[edit | edit source]
Discovery of radioactivity allowed for important breakthroughs in clinical medicine, especially in the fields of medical imaging and cancer treatments, increasing the scope of medical diagnoses and therapies. There are different techniques used for medical imaging, such as Scintigraphy, SPECT, and PET. Scintigraphy creates two-dimensional pictures. SPECT (single photon emission computed tomography) and Positron emission tomography (PET scan) form three-dimensional pictures. These nuclear medical images are generally more organ, tissue or disease specific than other techniques, like CT or X-rays. Furthermore they are used to follow metabolic processes of the body and do not only show the anatomical structure of an organ. Cancer treatment involving radioactivity is based on irradiating a tumour in the body. The high energy radiation then interferes with the tumour cells, damaging its DNA, which stops the cell proliferation. Unfortunately this method has proven to be dangerous for the patients as cells around the tumour were also irreversibly damaged, so new methods of tumour therapy are currently being investigated, such as proton therapy.
Literature review[edit | edit source]
Radioactivity is used in medical imaging. Medical imaging also allows to monitor metabolical processes, circulatory system or our immune system, which provides another view into patient’s body, and allows for early treatment of pathological conditions, such as arteriosclerosis. Using radioactivity to visualise patient’s body means exposure to ionising radiation, but thanks to modern technology it is possible to decrease the amount of radiation emitted by using more sensitive detectors. Method by which imaging methods such as Scintigraphy, SPECT, or PET scan work is by utilising radioactive substances or radioactivity in a variety of ways. In the three techniques a tracer substance (radiopharmaceutical), which contains a γ ray emitting isotope, which is later indigested or injected into the patient’s body. The patient is then screened using a sensor that detects the incoming γ radiation and its direction, and finally an image of the patient’s body can be created by using a computer. In Scintigraphy the detector detects radiation only from above, unlike SPECT or PET scan where the detector is circular around the patient. The advantage of PET over SPECT is that less tracer substance is required, because most radiation is detected. Whereas in SPECT only 0.0001% of the emitted protons are detected, in PET scan the detection of radioactivity is 100-fold increased. The reason is the collimator, used for SPECT for detecting the direction of the emitted protons. With this techniques it is possible to see the process of metabolising the radiopharmaceutical in an organ. If parts of the organ works slower than normally, it could show a disfunction. If the metabolism is increased it could show a tumour or hyper-function. Regarding tumour treatment, use of gamma rays has been successful, but the treatment doesn’t have high success rate, and the possibility of side effects is substantial. Especially dangerous is irradiation of neighbouring cells which gets damaged by the ionising beams. This can cause mutations of DNA of the cells possibly resulting in uncontrolled proliferation, thus creating another tumour. But the advantages of tumour therapy seem to outweigh the disadvantages, but it is important to note that other treatment methods are jut being investigated. Some have already gone into clinical trial. Therefore for the time being we have to settle with radiation therapy as other method are either very limited or non-existent whatsoever. Regarding ethics, it is required to have the patient’s voluntary consent before using imaging methods or tumour treatment based on radioactivity as some people do feel threatened when faced with radioactivity. Therefore the amount of radiation a patient is exposed to must not exceed the amount routinely required for scan or tumour treatment as that could harm the patient’s body.
Apparatus [edit | edit source]
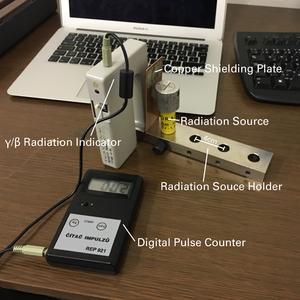
- Radiation source
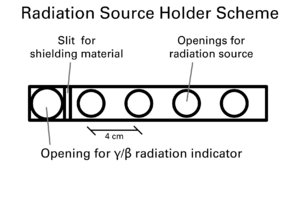
- Radiation source holder
- γ/β radiation indicator
- Digital pulse counter
- Copper plate shield (50 x 100 x 2 mm)
- Aluminium plate shield (50 x 100 x 2 mm)
- Iron plate shield (50 x 100 x 2 mm)
Methodology[edit | edit source]
- Connect the digital pulse counter with the γ/β radiation indicator using the provided lead and turn both pieces of equipment on
- Set the γ/β radiation indicator into the biggest hole of the radiation source holder, so that it is at 90° degrees to the long axis of the radiation source holder
- Make sure that the radiation source is closed by its outer ring and take it to a different room in order to prevent systematic error in radiation background reading
- Press the 100s button on the digital pulse counter to gather background radiation data and note the values. Repeat 10 times.
- Bring the radiation source back, secure it in the hole closest to the γ/β radiation indicator in the holder, and open it so that β radiation is being emitted.
- Press the 10s button on the digital pulse counter and note down the values. Repeat 5 times
- Repeat step 6 for the rest of the holes present in the holder, which are 4cm apart.
- Repeat step 6 & 7, but instead using γ radiation
- Secure aluminium plate shield in the holder, and take five 10s measurements from each distance of the holder using β radiation, then γ radiation, note down the values
- Repeat step 9 for copper plate shield and then iron plate shield
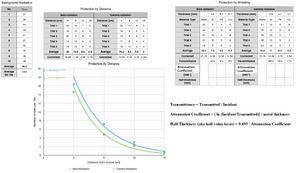
- In order to calculate the background radiation, average all gathered data and divide by ten to get final correction result per 10 seconds
- In order to calculate protection by shielding for each given material, average the 10s results and subtract background radiation result per 10s. Repeat for every materials and both types of radiation
- In order to calculate protection by distance, average the 10s results for each distance and subtract the background radiation per 10s. Repeat for every distance and both types of radiation
- CALCULATE (a) THE TRANSMITTANCES FOR THE GIVEN THICKNESS OF EACH MATERIAL (a) THE ATTENUATION COEFFICIENT OF EACH MATERIAL AND (c) THE HALF-THICKNESS (also known as) HALF-VALUE-LAYER (HVL) OF THE MATERIAL USING THE EQUATION I = Io e-ux WHERE u IS THE ATTENUATION COEFFICIENT. ATTENTION!!! - THE CALCULATIONS BELOW ARE NOT ALL CORRECT.
Conclusion[edit | edit source]
Nowadays cancer treatment is moving towards using proton therapy, which is possible to be focused more precisely onto the tumour by using magnetic field, resulting in unharmed surrounding tissue. Another highly beneficial addition is medical imaging, which allows early diagnosis of pathological conditions. Screenings are safer for the patient than exploratory surgery even with the use of radioactive substances. Early diagnosis significantly increases chances of successfully treating patient. Strong magnetic fields have a big future in medicine, e.g. combining PET with MRI. PET detector could be integrated into MR system, thus it can be operated just within the conventional MR system. The advantage is that both techniques can supplement each other, decreasing radiation dose. In comparison to PET-CT, not only the radiation dose is decreased, but also the contrast of soft tissue is better. Uses are for example diagnosis of dementia and screening of either the whole body and local parts.
Bibliography[edit | edit source]
- CancerResearchUK. (N.D.). "Our research on clinical trials and new treatments." Retrieved 6.12.2016, from http://www.cancerresearchuk.org/our-research/our-research-by-cancer-subject/our-research-on-clinical-trials-and-new-treatments.
- David J. Brenner, C. D. E. (2004). "Estimated Radiation Risks Potentially Associated with Full-Body CT Screening." Retrieved 6.12.2016, from http://pubs.rsna.org/doi/abs/10.1148/radiol.2323031095.
- Vetter, R. J. (2014). "Ethics of Radiation Protection in Medicine." Retrieved 6.12.2016, from http://hps.org/documents/medicine_ethics_vetter.pdf.
- PD Habib Zaidi, Ph.D.(N.D.) Geneva University Hospital, Division of Nuclear Medicine, CH-1211 Geneva, Switzerland, from http://www.sciencedirect.com/science/article/pii/S0939388915701790