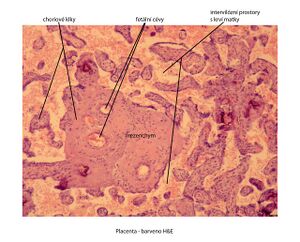
Placenta (histology)
Placenta (placenta discoidea, haemochorialis et cotyledonata)
Basic characteristics[edit | edit source]
- communication and barrier interface between two separate organisms
- bowl shape (diameter 20 cm), maximum thickness up to 3 cm
- divided by septa into 15–20 individual incompletely separated placental segments – cotyledons
- the embryo envelopes: chorion and trophoblast are involved in its formation
- chorion – mesenchymal tissue and trophoblast
- trophoblast - one of the first tissues that arises during the development of the embryo, it is divided into cytotrophoblast - made up of cells with preserved mitotic activity and syncytiotrophoblast - the character of the cells
- amnion – mesenchymal tissue, covered by single-layer flat to cubic amniotic epithelium
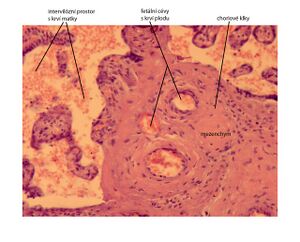
We recognize: pars materna placentae, pars foetalis placentae. Between the two plates there is an intervillous space (filled with maternal blood), the inner surface of this space is lined with a layer of syncytiotrophoblast.
Pars materna placentae (maternal part) – a derivative of the mucous membrane[edit | edit source]
- it originates from the plate of the transformed stroma of the uterine mucosa, the so-called decidua basalis; the decidua is formed within a few days under the influence of progesterone from the pseudodecidually changed tissue of the endometrial stroma in the secretory phase
- decidua basalis characterized by the presence of large spherical decidual cells - scattered in a sparse collagenous tissue, they contain many glycogen and lipid inclusions (with the secretion of the endometrial glands, they represent the first source of nutrients for the implanting embryo)
- the growth of the trophoblast causes pressure on the endometrium, including its arteries, which react by changing their arrangement until the bead-like - dilated terminal arterial branches serve as a buffer reservoir (to maintain the balance of blood pressure in the placenta), they open freely into the intervillous space (volume about 150 ml, maternal blood changes about 3x to 4x per minute)
- the decidua basalis sends out septa, they do not divide the intervillous space completely (they do not grow to the opposite chorion plate), but they functionally divide the individual cotyledons
The connection between the maternal and fetal parts of the placenta is strengthened by stem villi (i.e. anchoring or attachment), they have the ability to contract - by pulling the maternal part of the placenta, they regulate the lumen of the outlet of the supply artery to the cotyledon (thereby the fetus also actively participates in the regulation of blood flow through the placenta).
Pars foetalis placentae (fetus part)[edit | edit source]
- formed by the chorionic plate (thin collagen tissue, originating from the extraembryonic mesoderm), from which the chorionic villi depart
- stem villi, which form the center of the cotyledon one by one, further branch into mature and immature intermediate villi
- immature intermediate villi are terminated by many thermal villi, where the most efficient exchange of blood gases (between maternal and fetal blood) occurs
- immature intermediate villi are terminated by mesenchymal villi
- the surface of the chorionic plate and villi is initially covered by a layer of mitotically active cytotrophoblast and surface syncytiotrophoblast, later the layer of cytotrophoblast becomes discontinuous and below the layer of syncytiotrophoblast we find cytotrophoblast in the form of isolated Langhans cells
- syncytiotrophoblast nuclei are very often accumulated in groups forming nodules
- the stroma of the villi first has the character of mesenchymal tissue, later also a sparse collagenous tissue matures, in which there are numerous large spherical macrophages, Hofbauer cells
- vessels of the villi lose the tunica adventitia, in the terminal villi they are already formed only by capillary sinusoids
Fetoplacental circulation[edit | edit source]
- successor to the simpler embryochoric circulation
- secured by two umbilical arteries (they bring deoxygenated blood from the fetus), branches in the chorionic plate and enters the villi as blood capillaries, oxygenated blood returns to the fetus through the umbilical vein
Placenta - function[edit | edit source]
- ensures the exchange of metabolites and gases between maternal and fetal blood
- prevents the passage of certain substances and NOx
- serves as a temporary endocrine organ - production of hormones (HCG, chorionic somatotropin, estrogens in cooperation with the fetal adrenal cortex - supplies the precursor, sulfated dehydroepiandrostenedione, relaxin)
Placental barrier[edit | edit source]
First formed by:
- syncytiotrophoblast
- discontinuous cytotrophoblast
- trophoblast basal lamina
- layer of mesenchymal tissue
- basal lamina of the endothelium
- fetal capillary endothelium
As the placenta matures, the capillaries of the villi come into contact with the syncytiotrophoblast (similar to the blood-air barrier in the lungs).
Fibrinoid deposits[edit | edit source]
- deposits that limit the transfer of desirable substances, caused by the aging of the placenta
- fibrin from the intervillous space, tissue detritus and placental secretion
- Langhans fibrinoid – on the chorionic plate
- Rohr's fibrinoid – on the former cytotrophoblast envelope in the decidua basalis, especially in the attachment villi
- Nitabuch's fibrinoid – in the depth of the decidua basalis
In the first week after birth, the remnants of the decidua basalis leave in the form of lochia rubra.
Links[edit | edit source]
Related articles[edit | edit source]
- Placenta
- Placenta - histological preparations
- Atlas of histological preparations - female reproductive system
Source[edit | edit source]
- VAJNER, Luděk – UHLÍK, Jiří – NOVOTNÝ, Tomáš. Medical histology II : Microscopic anatomy. 1. edition. Prague : Nakladatelství Karolinum, 2012. 173 pp. ISBN 978-80-246-2165-4.