Patellofemoral syndrome
Femoropatellar disorder can be defined as muscle imbalance, pain, instability in the area of the extensor apparatus of the knee, but also as inflammation.
Etiology and clinical picture[edit | edit source]
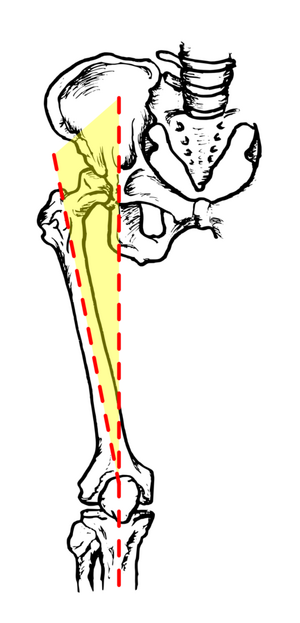
The exact etiology of this syndrome is unknown. However, the cause of the syndrome is mostly attributed to an increase in the Q angle.
It is the angle between the quadriceps femoris tendon and the patellae ligament. An angle greater than 20º causes activation of m. quadriceps femoris pulling the patella in a lateral direction and thus the formation of hyper-pressure of the patella on the lateral condyle of the femur.
Even with regard to the clinical picture, the authors differ in their opinion. According to one author, it is mainly a patient 20-45 years old, more often a woman, above average active, but it does not have to be an athlete. Other authors attribute this pain to adolescents, where it appears either spontaneously or with extreme loading of the cartilage. According to them, normally active adults are less susceptible, but morbidity increases with age, and in older patients the pain is caused by osteoarthritis. Another author claims that AKP (Anterior knee pain) syndrome can affect people of any age, but more often adolescents or young adults who do sports. The patient usually presents with pain under the patella, which occurs mainly when walking down stairs, down a hill, when squatting or when flexing the knee joint for a long time (traveling by car).
In conclusion, the patient's clinical condition may look like this:
- The pain originates only in the knee joint, not in the hip or lumbar region.
- Cruciate and collateral ligaments are not damaged or loosened.
- Physiological mobility of the tibiofemoral and proximal tibiofibular joints is normal and shows no signs of damage.
- The menisci are not damaged.
Diagnostics[edit | edit source]
During the examination, we obtain anamnestic data, we also perform an "aspect examination", where we evaluate the configuration of individual parts and overall motor skills. This examination is followed by a "palpation examination", which allows us to find out the muscle tone, trophic level, consistency and location of the adhesion pain. It is also important to find out the "range of motion", both passive and active, as well as "muscle shortening and strength".
In addition to physiotherapeutic methods, arthroscopic examinations are used, which are among the most accurate examination methods. X-ray, where the shape, position or hyperpression of the patella is checked with special projections, and sonographic examination.
All tests are based on the occurrence of pain due to increased pressure on the affected articular surface of the patella. These tests include the examination of femoropatellar pain, Zohlen's sign, plane sign, Fründ's test, Insal's test, Fairbank's Apprehension Test, tuning fork test, Hyperpressure Test, examination according to Wilson, etc.
Examination of femoropatellar tenderness[edit | edit source]
The examined person lies on his back and his knee is in extension. We palpate the articular surfaces of the patella. We then deflect the patella laterally and then medially, while palpating the lateral and medial facets. Deviation below 5 mm means shortening of the patella suspension apparatus, deviation above 2/3 of the patella surface means hypermobility of the patella.
Zohlen's Sign[edit | edit source]
The patient lies supine with the knee in full extension. The examiner presses on the tendon of the quadriceps femoris muscle, which is located above the base of the patella, and the patient performs an isometric contraction of this muscle. If pain is induced, the test is positive.
Planer sign[edit | edit source]
In the same position as the Zohlen test; we push the patella towards the joint and move it proximally and distally. This again can cause pain.
Fründ's test[edit | edit source]
The examiner taps the patella at 90° flexion.
Insal Test[edit | edit source]
The test is similar to the planer sign. We press on the patella, but move it medially and laterally.
Fairbank's Apprehension Test[edit | edit source]
We test for patellar dislocation. The patient lies with the knee extended and the surrounding muscles relaxed. The examiner attempts to recreate the dislocation by sliding the patella laterally, and the patient is then instructed to flex the knee. If the test is positive, the dislocation occurs in the extension or initial flexion phase of the knee.
Tuner Fork Test[edit | edit source]
Place the tuning fork on the patella. The test is positive if the patient perceives the vibration for a shorter period of time than a patient with a healthy knee.
Hypertension Test[edit | edit source]
If the femoropatellar cartilage is damaged, the patient feels pain when the patella is compressed against the femur.
Investigation according to Wilson[edit | edit source]
The patient lies on his back and the examiner flexes his knee to 90° and strongly inwardly rotates the lower leg. It still keeps the tibia in internal rotation and slowly extends the knee. The test is positive if there is pain in flexion around 30° and if it disappears with violent internal rotation of the lower leg. The pain is explained by internal rotation of the lower leg in flexion of around 30°, and the tuberculum mediale eminentiae intercondylaris comes into contact with the medial condyle of the femur in the area of the cartilage lesion.
Rehabilitation[edit | edit source]
Therapy should be chosen according to the identified problems, taking into account the patient's age and condition. Exercise has a certain character and is very individual.
The goal of therapy is:
- maintain full range of motion in the knee joint
- prevent atrophy of the quadriceps femoris muscle
- strengthen muscle mass in the full range of motion
- maintain mobility of the patella
- strengthen the entire locomotion apparatus (even the upper limbs for possible support)
The treatment can also be described in six points
- The first important step is to remove the effusion in the knee. Limitation of the function of the quadriceps femoris muscle can cause even a 20 ml effusion. For this, DD – CP currents or cryotherapy can be used from physical therapy.
- We also try to eliminate pain, the cause of which may be patellar hyper-pressure or effusion. From kinesiotherapy, soft tissue technique, traction of the knee joint, mobilization of the head of the fibula or mobilization of the patella are used. From physical therapy, electrotherapy is chosen, for example, ultrasound for the quadriceps femoris muscle. And last but not least, the femoropatellar joint is relieved with the help of orthoses and taping.
- Next, we focus on the extensibility of soft structures, where it is mainly about restoring the mobility of the medial and lateral reticulum, the mobility of the upper and lower pole of the patella and the mobility of the iliotibial tract.
- One of the most important points is individual exercise focusing on improving muscle activation, especially the vastus medialis muscle.
- We use plyometric and sensorimotor training to improve proprioception.
- The last task is to improve the biomechanical conditions in the knee area, thanks to taping or orthoptic support.
References[edit | edit source]
- KOLÁŘ, Pavel. Rehabilitace v klinické praxi. 1. edition. Galén, 2010. 713 pp. ISBN 978-80-7262-657-1.
- TRNAVSKÝ, Karel – RYBKA, Vratislav. Painful knee syndrome. 1. edition. Galén, 2006. 225 pp. ISBN 80-7262-391-5.
- THEUEROVÁ, Šárka. Etiology and diagnosis of femoropatellar pain syndrome. Olomouc, 2003,