Oral glucose tolerance test
The oral glucose tolerance test (OGTT) reflects the body's response to glucose in a physiological way and assesses whether the body is able to maintain blood glucose levels within the normal range after glucose exposure. It is a summary of information not only about the effects of hormones regulating glycemia, but also about processes in the gastrointestinal tract (rate of gastric emptying, intestinal passage and resorption) and liver function.
The oral glucose tolerance test is used primarily for the early diagnosis of gestational diabetes. In this case, it is used as a routine screening examination, performed on all pregnant women at the turn of the second and third trimesters (at high risk, in addition, as soon as possible after pregnancy).
In others, the oral glucose tolerance test is recommended as an additional diagnostic test for the diagnosis of DM if fasting and random glucose values cannot be determined (especially if fasting blood glucose is between 5.6 - 7.0 mmol/l). If fasting or random blood glucose levels are conclusive for the diagnosis of DM, OGTT would be an unnecessary burden for the patient and is therefore contraindicated. Furthermore, it is not performed in acutely ill and immobilized patients or in patients on a reduction diet.
Performing an oral glucose tolerance test[edit | edit source]
- 3 days before the test we do not limit the intake of carbohydrates (at least 150 g/day) and the patient performs the usual physical effort
- after fasting for 8-14 hours, a fasting blood sample is taken;
- the patient drinks 75 g of glucose dissolved in 250-300 ml of tea or water within 5-10 minutes;
- the patient remains seated and does not smoke during the examination;
- another blood sample is taken from pregnant women at 60 and 120 minutes, from all other patients only at 120 minutes after glucose exposure.
In addition to the above-mentioned oGTT method, an even more detailed so-called glycemic curve can be performed, where blood is taken several times, usually at 30-minute intervals.
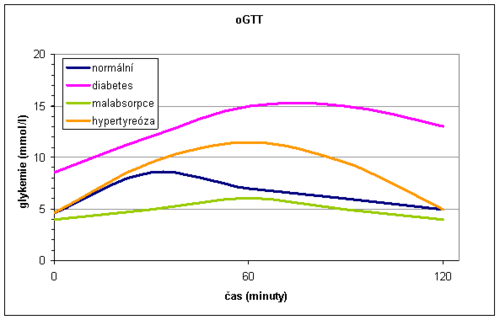
During the glycemic curve we can describe three sections:
- Glucose administration orally absorbed in the intestine and blood glucose increases - the rising part of the glycemic curve. It is usually steep after gastrectomy and flat during malabsorption. As the blood glucose increases, the oxidation of glucose in the muscles is stimulated and glycogen is formed in the liver.
- The function of the liver and the effects of insulin in the liver are reflected by another - the peak part of the glycemic curve. In the onset of DM , glucose in the liver is not sufficiently converted to glycogen, and therefore the peak of the glycemic curve exceeds 11.1 mmol/l and the maximum occurs later than in 60 minutes. In liver disease , the apex of the curve is also altered. Hepatocytes are not enough to metabolize the absorbed glucose, so more glucose passes into the periphery. The peak also exceeds 11.1 mmol/l and the increase persists for more than 60 minutes, but unlike DM, it returns to normal at 120 minutes (bell shape of the curve). In hyperthyroidism, the level of 11.1 mmol/l is also exceeded due to rapid absorption, but the decrease is rapid (gothic curve shape).
- The descending part of the glycemic curve is dependent on the effects of insulin and is physiologically characterized by a decrease in glucose levels. A slow and insufficient return of blood glucose to normal is a classic manifestation of DM
Normally, we observe a maximum rise in 30-60 minutes, there is no glycosuria and after 2 hours the blood glucose returns to fasting values.
In general, the oGTT is burdened with a large random error and low reproducibility.
Evaluation of blood glucose and OGTT[edit | edit source]
Healthy individuals have fasting plasma glucose <5.6 mmol/l, with oGTT having a fasting blood glucose <7.8 mmol/l at 120 minutes. It testifies to the diagnosis of DM:
- fasting blood glucose> 7.0 mmol / l
or
- random blood glucose> 11.1 mmol / l
or
- glycemia> 11.1 mmol / l at 120 minutes OGTT
together with classic clinical symptoms (thirst, polyuria, weight loss).
To confirm the diagnosis of DM, a re-examination from the next collection on one of the following days is required.
Links[edit | edit source]
Sources[edit | edit source]
- Doporučený postup. Diabetes mellitus - laboratorní diagnostika a sledování stavu pacientů. 2015. Dostupné také z URL <http://www.cskb.cz/res/file/doporuceni/DM/DM_dop_201601.pdf>.
- ↑ Doporučený postup. Dooručené diagnostické a terapeutické postupy pro všeobecné praktické lékaře. 20ěé. Dostupné také z URL <https://www.svl.cz/files/files/Doporucene-postupy/2020/DIABETES-MELLITUS-2020.pdf>.