Optical apparatus of the eye, oculomotor muscles, eye movements
The eye consists of: cornea, conjunctiva, aqueous humor, lens, vitreous. We recognize two axes in the eye - visual (pointing through the center of the lens to the fovea) and optical (pointing through the center of the lens to a place about 5° [1] away from the fovea to the left of the right eye and to the right of the left eye).
- Basic data [1]
- Perceived light: 400 to 700 nm;
- Intraocular pressure: 2.0 to 2.9 kPa (15 to 22 torr);
- Refractive power of the lens: the reciprocal of the focal length in meters, i.e. 1 D corresponds.
Optical apparatus of the eye[edit | edit source]
The eye contains a light-refracting and light-receiving apparatus. The refracting apparatus consists of the cornea and the lens, as well as the aqueous humor and vitreous humor. The optical power of the unaccommodated eye is approximately + 59 D, of which 43 D belongs to the cornea and 16-20 D to the lens. The optical power of the lens is variable. During accommodation, the eye does not have an optical power of 59 D.
Visual axis of the eye[edit | edit source]
The visual axis of the eye is a straight line that connects the optical center of the eye with the yellow spot. It makes an angle of about 5° with the optical axis of the centered system of the eye, that is, the yellow spot is not in the image focus of the eye, but is deviated from it by about 1.5 mm temporally.
Cornea[edit | edit source]
The cornea is approximately spherical in shape. It separates the internal environment of the eye from the surrounding air environment (with a refractive index of 1), which makes it the most efficient of the entire refractive system. The refractive index of the cornea is 1.37.
Lentil[edit | edit source]
The lens is a crystal clear structure whose optical power is variable due to its accommodation capacity. Due to the heterogeneous structure of the lens, there is no uniform index of refraction. For practical purposes, only the average refractive index of the whole lens of 1.42 is used. The passage of the ray through the lens is therefore not straight.
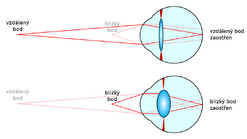
The ciliary apparatus, on which the lens is suspended, has the ability to mechanically change the curvature of the front and back of the lens, thereby changing its optical power. When looking up close, muscle contractions loosen the fibers of the suspensory apparatus of the lens, it bulges and its refractive index increases.
Accommodation ability of the lens[edit | edit source]
The range of accommodation ability of the lens is determined by the so-called near and far points.
Near point[edit | edit source]
The near point (punctum proximum) is the nearest point that the eye sees sharply at maximum accommodation. With age, the elasticity of the lens decreases and therefore the accommodation capacity, and the near point moves away. In a ten-year-old child, the accommodative width is about 15 D and the near point is 7 cm in front of the eye. In a 20-year-old person, an emmetrope, the accommodative width is reduced to 10 D (the near point is 10 cm in front of the eye). In an adult younger person, an emmetrope, it is at a distance of 25 cm in front of the eye (accommodative width 4 D), which is the so-called conventional visual distance. When the near point gets over 25 cm in front of the eye, problems with near accommodation begin to appear, especially when reading. This defect is called presbyopia. Around the age of 70, the lens loses its ability to accommodate and the accommodation width is 0 D.
Far point[edit | edit source]
The far point (punctum remotum) is the farthest point that the eye can see clearly without accommodation, and in a healthy eye it is at infinity (practically, we consider a distance of 5 m as infinity for the eye).
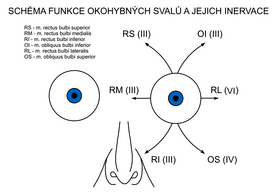
Oculomotor muscles - movements of the eye[edit | edit source]
The oculomotor muscles are the muscles that ensure the movements of the eyeball.
According to the course of the muscle bundles, we divide them into:
- direct,
- oblique.
The common origin of the oculomotor muscles is a circular tendon located at the tip of the orbit - anulus tendineus communis.
Musculi recti[edit | edit source]
Attachments of individual muscles are located in each quadrant of the bulb. The name corresponds to the position of the muscle.
The third cranial nerve – the oculomotor nerve provides innervation to all rectus muscles, with the exception of the rectus lateralis muscle, which already falls under the abducens nerve.
- m. rectus superior: n. III.;
- m. rectus inferior: n. III.;
- m. rectus medialis: n. III.;
- m. rectus lateralis: n. VI..
Musculi obliqui[edit | edit source]
The oblique muscles have a common beginning with the rectus muscles, but their attachments and courses are different.
Innervation is provided by the trochlearis nerve and the oculomotor nerve.
- m. obliquus superior: n. IV.;
- m. obliquus inferior: n. III..
Oculomotor muscle and its function[edit | edit source]
| Nerve | Innervated muscles | Physiological function | ||||
|---|---|---|---|---|---|---|
| III - the oculomotor nerve | parasympathetic part | m. sphincter puppilae, m. ciliaris | narrowing of the pupil, accommodation | |||
| motor fibers | m. rectus medialis, superior et inferior, m. obliquus inferior | movement of the eye nasally, up, down | ||||
| m. levator palpebrae superioris | lid elevation, open eye slit | |||||
| IV - the trochlearis nerve | m. obliquus bulbi superior | movement of the bulb down and out | ||||
| VI - the abducens nerve | m. rectus lateralis | abduction of the eye | ||||
| sympaticus | m. dilatator pupillae, m. tarsalis | pupil dilatation, eyelid tone | ||||
Links[edit | edit source]
Related articles[edit | edit source]
References[edit | edit source]
Bibliography[edit | edit source]
- TROJAN, Stanislav. Lékařská fyziologie. 4., přeprac. a uprav edition. Praha : Grada Publishing, a. s, 2003. 772 pp. ISBN 80-247-0512-5.
- KYMPLOVÁ, Jaroslava. Katalog metod v biofyzice [online]. [cit. 2012-09-20]. <https://portal.lf1.cuni.cz/clanek-793-katalog-metod-v-biofyzice>.
- PETROVICKÝ, Pavel. Anatomie s topografickými a klinickými aplikacemi. 1. edition. Martin : Osvěta, 2002. 542 pp. vol. 3. ISBN 80-8063-048-8.