Mamma - description and structure, blood supply and innervation, lymphatics
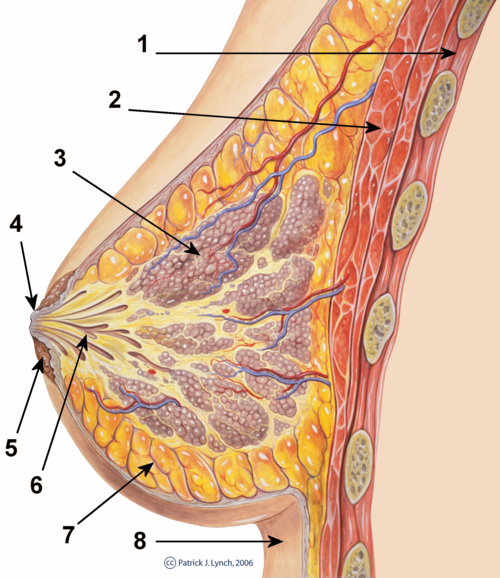
Description and structure[edit | edit source]
The breasts are paired structures that are located on the anterior thoracic wall, in the pectoral region, present in both male and female.
In females, the breasts contain the mammary glands, which are accessory glands of the female reproductive system.
They are exocrine, modified apocrine glands
They are structurally dynamic, which means they change with the womans age, menstrual cycle and reproductive statues. They have 15-20 secretory lobes which are separated via fibrous bands known as suspensory ligaments of the breast. The lobes contain locules comprised of tubuloalveolar glands. The glands drain to the ducts of these lobes , known as the lactiferous ducts , which open into the nipple.
Glandula mammae[edit | edit source]
- the largest skin gland
- mamma - breast - is a bulge on the front wall of a woman's chest containing the ‘’'glandula mammae'‘’' - mammary gland
- several anthropological shape types:
- mamma disciformis - flat, low, bowl-shaped
- mamma sphaeroidea - hemispherical, classic, only transiently
- mamma piriformis - pear-shaped, beginning to form sulcus inframammalis underneath
- mamma pendula - flaccid
- skin pale and thin, subcutaneous veins shining through, richly innervated
- areola mammae - the mammary areola, larger in pregnancy
- around the areola there are small bumps with glands - glandulae areolares (Montgomeryi)
- papilla mammae - breast nipple - usually slightly raised, sometimes slightly depressed
- ductus lactiferi - mouth at the tip of the papilla, coming from deep within the gland
- area cribriformis papillae - 15-20 holes at the tip of the papilla, outlet of ductus lactiformis
- the papilla has its sebaceous glands, which protect its skin from maceration by milk and saliva infant
- there is smooth muscle in the areola, it runs radially (helically in the papilla)
Premammary fat
- flattens the pits (fossulae adiposae) between the glandular lobules and rounds the surface of the breast
- ligg. suspensoria mammae - bands of subcutaneous connective tissue, fixing the gland to the superficial pectoral fascia
Retromammary fat
- thick layer in which the bursa retromammalis may occur in lactating women
Vasculature[edit | edit source]
The arterial supply of the breast is rich and varied, drawing from multiple sources to ensure adequate blood flow.
Branches of the Axillary Artery:
- Superior Thoracic Artery: Supplies the upper part of the breast.
- Thoracoacromial Artery: Provides branches to the pectoral region and the breast.
- Lateral Thoracic Artery: Particularly important for the lateral aspect of the breast.
- Subscapular Artery: Contributes to the blood supply of the breast and surrounding regions.
Branches from the Internal Thoracic (Mammary) Artery: These branches run along the sides of the sternum and provide medial mammary branches to the breast.
Perforating Branches of the 2nd, 3rd, and 4th Intercostal Arteries: These arteries pierce through the intercostal spaces and supply the deeper tissues of the breast.
Innervation:[edit | edit source]
The breast is innervated primarily by the intercostal nerves, providing sensory and autonomic innervation.
- Intercostal Nerves 2-6:
- Anterior Cutaneous Branches: These branches supply the skin over the medial aspect of the breast.
- Lateral Cutaneous Branches: These branches innervate the skin over the lateral aspect of the breast.
- Nipple Innervation:
- 4th Intercostal Nerve: Specifically, the nipple and areola receive sensory innervation from the anterior and lateral cutaneous branches of the 4th intercostal nerve.
Lymphatics:[edit | edit source]
The lymphatic system plays a crucial role in the drainage of the breast, and its understanding is needed, especially in the case of breast cancer.
- Subareolar Lymphatic Plexus:
- Collection Point: Lymph from the breast and nipples first collects into the subareolar lymphatic plexus.
- Primary Drainage Pathway:
- 75% of Lymph: The majority of lymph (approximately 75%) drains from the subareolar plexus into the pectoral lymph nodes.
- Pectoral to Axillary Lymph Nodes: From the pectoral lymph nodes, lymph travels to the axillary lymph nodes.
- Axillary to Subclavian Lymphatic Trunk: Finally, lymph from the axillary lymph nodes drains into the subclavian lymphatic trunk.
- Secondary Drainage Pathway:
- 25% of Lymph: The remaining 25% of lymph drains into the parasternal lymph nodes.
- Parasternal to Bronchomediastinal Lymphatic Trunk: The parasternal lymph nodes subsequently drain into the bronchomediastinal lymphatic trunk.
Clinical Significance:[edit | edit source]
Breast Cancer Staging: During the staging and treatment of breast cancer, axillary lymph nodes are often the first to be examined and potentially removed to check for metastasis, as they are a primary drainage site and can indicate the spread of cancer.
Structures associated with the mammary gland[edit | edit source]
Areola[edit | edit source]
A circular, pigmented area surrounding the nipple. It serves as a visually distinct region that becomes darker during pregnancy and lactation to help infants locate the nipple.
Nipple[edit | edit source]
The central raised structure within the areola containing the openings of the lactiferous ducts, which are channels through which milk is secreted during lactation.
Areolar Tubercles[edit | edit source]
Small elevations on the areola produced by the areolar glands, also known as Montgomery glands. These glands secrete an oily substance that lubricates and protects the nipple and areola during breastfeeding.
Suspensory Ligaments of the Breast (Cooper's Ligaments):[edit | edit source]
A fibrous network that inserts into the pectoral fascia and dermis over the skin of the breast. These ligaments provide structural support to the breast, maintaining its shape and anchoring it to the chest wall.
Histological structure of the mammary gland[edit | edit source]
- composed of 15-20 compound tuboalveolar glands - each gland forms a separate lobe
- individual lobes are separated by dense collagenous connective tissue and fatty tissue
- the axis of each lobe is the lobar duct (ductus lactiferus) - as the terminal part it extends into the sinus lactiferus - this narrows in the nipple area and exits to the surface as the porus lactiferus (diameter 0.5 mm)
- ductus lactiferus branches into interlobular ducts
Epithelial cells
- in the ductus lactiferus two-layered cuboidal or cylindrical epithelium, basal cells are composed of myoepithelial cells
- the ductus lactiferus is lined with multilayered squamous epithelium before the outlet
- in interlobular ducts single-layered cuboidal epithelium on well-developed basal lamina, discontinuous layer of myoepithelial cells
Changes due to age and functional status of the gland
- pre-pubertal mammary gland consists of the ductus lactiferi and a pair of interlobular ducts
- during puberty further branching of the ductus lactiferi and interlobular ducts → these give rise to the intralobular ducts - these form the basis of the lobules, lobules are typical structures of the adult female mammary gland, they are encased in sparse collagen ligament, they are separated by a denser ligament with collagen fibres
- during pregnancy cell proliferation occurs at the end of the terminal intralobular ducts → formation of alveoli, alveolar cells become secretory cells (developed granular endoplasmic reticulum, Golgi complex, numerous mitochondria, lipid droplets, secretory vacuoles), each alveolus is surrounded by 4-6 myoepithelial cells (between secretory cells and basal lamina)
- during pregnancy milk is produced by alveolar cells, collects in lumina of alveoli and in lumina of ductus lactiferi, plasma cells increase around alveoli - pruduction of hl. IgA, lipid droplets increase in secretory cells - secreted apocrinally and casein and alpha-lactalbumin present in secretory vacuoles - secreted eccrinally
- after the end of lactation most alveoli degenerate, myoepithelial cells and basal lamina do not degenerate (for further pregnancy)
- after menopause' gland involution, atrophy of secretory compartments and ducts
References[edit | edit source]
Salvador notes
- KONRÁDOVÁ, Václava – UHLÍK, Jiří – VAJNER, Luděk. Funkční histologie. 2. edition. H & H, 2000. 291 pp. ISBN 80-86022-80-3.
- ČIHÁK, Radomír. Anatomy 3. 2. edition. Grada Publishing, 2004. 692 pp. ISBN 978-80-247-1132-4.