Inflammation of the stomach (Gastritis)
Inflammation of the stomach (gastritis) is defined as the inflammation of the gastric mucosa. Gastritis can be an acute or chronic condition.
Acute gastritis[edit | edit source]
Acute gastritis is defined as an acute inflammatory process that manifests itself in various forms of gastric mucosal involvement from hyperemia to erosion and ulcers. These alterations may cause acute gastrointestinal bleeding. Acute gastritis is transient and but could progress to chronic inflammation.
Pathogenesis[edit | edit source]
Although the mechanism of acute gastritis is not entirely clear, the following factorscontribute to the etiology:
- large doses of non-steroidal anti-inflammatory drugs, such as aspirin
- excessive alcohol consumption
- smoking
- cytostatics
- systemic infections (for example salmonellosis)
- uremia
- severe stress conditions (for example trauma, burns, conditions after surgical operations)
- ischemic injury and shock
- ionizing radiation
- mechanical trauma (for example nasogastric intubation)
- inappropriate diet (especially animal fats and spices)
Morphology[edit | edit source]
- Acute gastritis can be localized or diffuse and appears macroscopically from simple mucosal congestion to erosion.
- Hemorrhage and erosion can be observed with an endoscope, this condition is known as acute erosive gastritis.
- Microscopically, the mucosa is congested and edematous
- Epithelial regeneration is evident in the gastric pits.
- If the cause disappears, acute gastritis heals within a few days with complete recovery of the gastric epithelium. If the cause persists, the inflammation may become chronic.
The clinical picture[edit | edit source]
Acute gastritis can be completely asymptomatic or with only mild symptoms, such as nausea, pain, vomiting or hematemesis (vomiting blood), but fatal blood loss could also occur. Acute gastritis is one of the main causes of hematemesis , especially in alcoholics.
Therapy[edit | edit source]
Therapy for acute gastritis could include the following:
- Dietary measures, rehydration, gradual realimentation
- Analgesics with antispasmodic effects (e.g. metamizole-pitophenone-fenpiverine , butylscopolamine ) can be used for colic abdominal pain; in nausea antiemetics (metoclopramide ); antidiarrheal drugs for diarrhea (eg chloroxine ), or probiotics.
Chronic gastritis[edit | edit source]
Chronic gastritis is defined as the presence of chronic inflammatory changes in the mucosa that can result in mucosal atrophy and epithelial metaplasia. Erosion is not usually present, as is the case with acute gastritis. It is noteworthy that different types of histological variants of chronic gastritis typically occur in different parts of the world.
Pathogenesis[edit | edit source]
The most important etiological association is Helicobacter pylori infection. This organism is a common pathogen with the highest incidence in developing countries. In areas where the infection is endemic, permanent carriers are demonstrated. Most carriers suffer from associated asymptomatic gastritis.
Types of chronic gastritis[edit | edit source]
From a morphological point of view, it is possible to distinguish: superficial or deep gastritis - differentiation according to the level of mucosa reaching the lymphoplasmocellular infiltrate
- Superficial gastritis is the mildest form of chronic gastritis, in which there are small alterations of the mucosa;
- Atrophic gastritis with loss of gastric glands - partial or complete - the most severe form of atrophic gastritis, in which gastric gland cells are replaced by mucus cells
- Atrophic gastritis with intestinal metaplasia - replacement of the gastric epithelium by the intestinal mucosa with goblet, Paneth cells and enterocytes - may be complete or incomplete ( precancerous lesions ).
From the etiological point of view, it is possible to distinguish:
- Type A - Autoimmune (antibodies against parietal cells and internal factor) - affects the body of the stomach
- A rarer form of chronic gastritis is autoimmune gastritis , which is caused by both the immunotoxic effect of lymphocytes damaging parietal cells and the production of antibodies against parietal cells of the gastric mucosa.
- Autoimmune damage leads to destruction and atrophy of the gastric epithelium with concomitant loss of hydrochloric acid and intrinsic factor produced by parietal cells. Internal factor deficiency can then result in pernicious anemia and achlorhydria.
- We find hypergastrinemia.
- This type of gastritis typically affects the body's stomach, where the main and parietal cells are located.
- Autoimmune gastritis occurs in areas of Scandinavia and is associated with other autoimmune diseases such as Hashimoto's thyroiditis and Addison's disease.
- Type B - Bacterial ( Helicobacter pylori infection ) - affects the antrum of the stomach
- This type of chronic gastritis results from the action of enzymes colonizing H. pylori bacteria and the release of harmful chemical compounds by neutrophilic granulocytes.
- The actual mucosal damage is of two types. On the one hand, there is a high production of hydrochloric acid, which poses a risk of duodenal ulcer , on the other hand, it affects the body and antrum (pangastritis) with mucosal epithelial atrophy, low production of hydrochloric acid and a high risk of adenocarcinoma.
Morphology[edit | edit source]
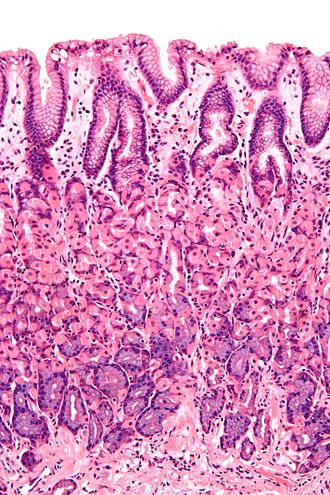
Regardless of the cause and type of chronic gastritis, microscopic inflammatory changes of the mucosa represent a lymphoplasmocellular infiltrate in the lamina propria occasionally accompanied by the presence of neutrophils.
Inflammation can be accompanied by loss of glands and mucosal atrophy, where the mucosa has a smooth surface. In these cases, we detect H. pylori bacteria nested in gastric mucus. The most prominent feature of the autoimmune type of gastritis is the loss of parietal cells.
Intestinal metaplasia means the replacement of the gastric epithelium by the intestinal mucosa with goblet, Paneth cells and enterocytes. Epithelial dysplasia can later occur until malignant adenocarcinoma .
The clinical picture[edit | edit source]
Chronic gastritis usually appears asymptomatic or with only mild symptoms such as stomach pain, nausea and vomiting. If there is a large loss of parietal cells in the autoimmune type of chronic gastritis, hypochlorhydria or achlorhydria as well as hypergastrinemia occurs.
- Patients with chronic gastritis caused by other causes may be hypochlorohydric, but since not all of their parietal cells have been destroyed, they may not develop achlorhydria or pernicious anemia.
- Chronic gastritis may be associated with peptic ulcer and gastric adenocarcinoma.
- In most patients who have peptic ulcer, the presence of infection has been demonstrated H. pylori. For these patients, the risk of gastric adenocarcinoma is up to five times greater than in the normal population.
- In the autoimmune type of chronic gastritis, the risk of adenocarcinoma is between 2 and 4%, which is slightly above the average in the normal population.
Therapy[edit | edit source]
Helicobacter pylori has to be eliminated if present, especially in the presence of an ulcer. Further therapy is mostly symptomatic. The treatment of autoimmune gastritis is unknown, vitamin B 12 substitution is recommended.
Source[edit | edit source]
References[edit | edit source]
- NEČAS, Emanuel. Patologická fyziologie orgánových systémů. Čast 2. 2. vydání. Praha : Karolinum, 2009. ISBN 978-80-246-1712-1.
- KUMAR, Vinay, Abul ABBAS a Nelson FAUSTO, et al. Robbins Basic Pathology. 8. vydání. Philadelphia : Saunders/Elsevier, 2007. 946 s. ISBN 978-1-4160-2973-1.
- KLENER, Pavel. Vnitřní lékařství. - vydání. Galén, 2001. 949 s. s. 460-462. ISBN 9788072621019.